Case Report
Multicentric Malignant Optic Nerve Glioma-A Rare and Challenging Diagnosis
Gunjan J, Shrivastava A*, Bhargavi P, and Singh Bains R
Department of Radiodiagnosis, MMIMSR, Mullana, Haryana, India
*Corresponding author: Amit Shrivastava, Department of Radiodiagnosis, MMIMSR, Mullana, Haryana, India.E-mail Id:dr.amitsrivastava@gmail.com
Article Information: Submission: 24/11/2023; Accepted: 15/12/2023; Published: 18/12/2023
Copyright: © 2023 Gunjan J, et al. This is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Optic nerve gliomas are predominantly benign tumors, commonly
arising in children and young adults. Malignant transformation is a
rare occurrence in optic nerve gliomas, and multicentric involvement
is even rarer. Herein, we present a case of multicentric malignant
optic nerve glioma to increase awareness of this uncommon variant
and contribute to the existing literature on optic nerve gliomas.
Case Presentation
A 44-year-old male presented with a 3-month history of
progressive bilateral visual loss. The patient complained of reduced
visual acuity, visual field defects in both eyes and color vision
impairment. On examination, afferent pupillary defects were noted
in both eyes. Visual field analyser revealed bitemporal hemianopia.
Fundus examination showed no evidence of disc edema. Visual
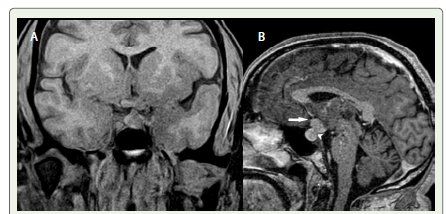
acquity at the time of presentation was 6/6. MRI revealed thickening
of the optic chiasma with altered T2/FLAIR hyperintense signal and
early post-contrast enhancement [Figure 1].
However, contour of optic chiasma was preserved. Pituitary
stalk and tuber cinerium were also thickened showing altered signal
intensity with intense post contrast enhancement. The lesions
demonstrated infiltrative growth patterns, resulting in fusiform
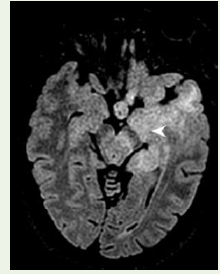
thickening of the intracranial parts of B/L optic nerves with mild
post contrast enhancement. Altered signal intensity was also seen
involving post chiasmatic left optic tract in the region of left temporal
lobe, left lateral geniculate body in the posterior part of thalamus with
involvement left hypothalamus, left hippocampus and left insular
cortex. No evidence of any hemorrhage/calcification/necrosis was
seen within it [Figure 2,3].
Figure 1: Coronal(A) and sagittal (B) T1W image shows thickened optic
chiasma (arrow) with thickened pituitary stalk (arrowhead).
Figure 2: Axial FLAIR image shows altered signal intensity in the region
of post chiasmatic left optic tract in the region of left temporal lobe,left
hypothalamus and left hippocampus.
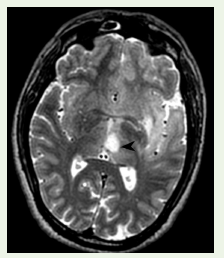
Figure 3: Axial T2W image shows a well-defined lesion in left thalamus
(arrowhead). On post contrast images, no enhancement was seen. This
lesion was described as a multicentric low grade glioma.
Another well-defined lesion appearing hyperintense on T2W/
FLAIR images, hypointense on TlW images, measuring approximately
1.2 x 2 cm was noted in left thalamus suggesting the multicentricity
of tumour. MRI with gadolinium contrast showed enhancement
in optic chiasma, pituitary stalk, tuber cinerium and intracranial
parts of bilateral optic nerves. Diffusion-weighted imaging (DWI)
and apparent diffusion coefficient (ADC) maps showed restricted
diffusion in the lesions, indicating high cellularity.
On the basis of MRI, differential considerations included bilateral
optic neuritis or multifocal hypothalamic chiasmatic optic nerve
glioma or metastatic disease. Rare possibility of lymphoma was also
considered after reviewing literature which seemed unlikely due to
the pattern of involvement.
The radiological findings were consistent with the diagnosis of
multicentric malignant optic nerve glioma.
Surgical interventions, histopathological examination of the optic nerve lesions are confirmatory in such cases. However, both of them could not be performed due to multicentric and infiltrative nature of the lesion making it a risky option when the risk versus benefit ratio was outweighed.
Surgical interventions, histopathological examination of the optic nerve lesions are confirmatory in such cases. However, both of them could not be performed due to multicentric and infiltrative nature of the lesion making it a risky option when the risk versus benefit ratio was outweighed.
Due to the multicentric nature of the tumour and involvement of
both optic nerves, complete surgical resection was not feasible. Poor
prognosis was explained to the patient. The patient refused to undergo
radiotherapy. Regular ophthalmological follow-up was scheduled to
monitor visual acuity and optic nerve function.
Discussion
Optic nerve gliomas are relatively benign when they occur in
childhood. Malignant gliomas of optic nerve are more common
in adulthood.The more common benign optic nerve glioma is
considered a low- grade astrocytoma and is frequently associated
with neurofibromatosis type [1]. Malignant optic glioma is a very rare
optic pathway tumor of the adulthood [2].
Optic nerve sheath is spared in optic neuritis and optic nerve
ischemia. In these conditions, there is diffuse enlargement of the optic
nerve. In conditions such as meningioma and pseudotumour, the
optic nerve is spared whereas the optic nerve sheath is enlarged.
[3,4].Those processes that involve both the optic nerve and sheath would
be favoured in the differential diagnosis of the lesion in this case.
Due to the extreme rarity and very rapid disease progression, the
point of origin cannot be certainly defined.[5] Secondary invasion
of the hypothalamus causes symptoms like polyuria and polydipsia.
[5,6] One report with computed tomography findings described a
case of malignant optic glioma of adulthood that extensively enlarged
the optic nerve but not the optic chiasm [7].
A syndrome of Optic nerve glioma in adults has been described
by Hoyt et al which is very similar to the case presented by us here [6].
In such cases, clinical examination does not favour optic nerve or intraorbital mass, rather due to optic nerve involvement, the diagnosis of optic neuritis is made and intravenous steroids are initiated. And if there is clinical improvement after initiation of steroids, the diagnosis is further stressed. But due to the rapid progression of the mass, there is rapid deteroiration in visual acuity which leads to unilateral blindness in rapid succession. Chiasmal involvement occurs in rapid progression suggested by bilateral reduced visual acuity and bilateral optic disk edema. The mass further progresses and invades the hypothalamus, basal ganglia, and internal capsule. Hypothalamic symptoms usually occur late in the clinical course. [5] There can also be lepto-meningeal and subpial spread of malignant optic glioma to the medial temporal lobes and brain stem. [7]The current case demonstrates spread of malignant optic glioma of adulthood to intracranial bilateral optic nerves, optic chiasma, pituitary stalk and post chiasmatic left optic tract.The multicentricity of the tumour was diagnosed as a lesion was seen in left thalamus. No other similar case has been found in literature.
In such cases, clinical examination does not favour optic nerve or intraorbital mass, rather due to optic nerve involvement, the diagnosis of optic neuritis is made and intravenous steroids are initiated. And if there is clinical improvement after initiation of steroids, the diagnosis is further stressed. But due to the rapid progression of the mass, there is rapid deteroiration in visual acuity which leads to unilateral blindness in rapid succession. Chiasmal involvement occurs in rapid progression suggested by bilateral reduced visual acuity and bilateral optic disk edema. The mass further progresses and invades the hypothalamus, basal ganglia, and internal capsule. Hypothalamic symptoms usually occur late in the clinical course. [5] There can also be lepto-meningeal and subpial spread of malignant optic glioma to the medial temporal lobes and brain stem. [7]The current case demonstrates spread of malignant optic glioma of adulthood to intracranial bilateral optic nerves, optic chiasma, pituitary stalk and post chiasmatic left optic tract.The multicentricity of the tumour was diagnosed as a lesion was seen in left thalamus. No other similar case has been found in literature.
Conclusion
Multicentric malignant optic nerve glioma is an extremely rare
variant of optic nerve glioma, with limited published reports. Its
diagnosis is challenging due to its rarity, variable clinical presentation,
and radiological features overlapping with other optic neuropathies.
The role of MR imaging plays a pivotal role in the early diagnosis of
this disease.
Treatment involves a multimodal approach, including surgical resection, radiation therapy, and chemotherapy, tailored to individual patients.
Treatment involves a multimodal approach, including surgical resection, radiation therapy, and chemotherapy, tailored to individual patients.