Review Article
Comparison of DHA Levels in Breast Milk of Indian Mothers of Term and Preterm Neonates
Mani B1*, Gonsalves R1, Rao S2, Mani I3, Bannikopa P3 and Janet V1
1St. John’s Medical College Hospital, Bangalore, India
2Department of Neonatology, St. John’s Medical College Hospital, Bangalore, India
3Department of Nutrition, St. John’s Research Institute, Bangalore, India
*Corresponding author: Mani B, St. John’s Medical College Hospital, Bangalore, India; E-mail: bhavupaveen@gmail.com
Article Information: Submission: 17/04/2022; Accepted: 23/05/2022; Published: 27/05/2022
Copyright: © 2022 Mani B, et al. This is an open access article distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objectives: Docosahexaenoic acid (DHA, 22:6 n-3) is a fatty acid, which plays an important role in growth and neurodevelopment. There is wide
variability of DHA levels in breast milk based on gestational age, geographical location, and diet. Indian diets contain low levels of DHA, implying lower breast
milk DHA levels. However there is dearth of information on the fatty acid profile of the breast milk of Indian mothers.
In this study we compared the fatty acid composition of the breast milk of Indian mothers with term and preterm neonates and determined the relationship
of breast milk DHA with dietary intake of DHA.
Study Design: This observational study included postnatal mothers (Days 4-7) from the NICU and postnatal wards of a tertiary care hospital in South
India. Expressed breast milk from 23 term and 24 preterm mothers was analyzed for fat composition by gas chromatography. Dietary history was taken by a
food record questionnaire. BMI of mothers was noted. The sample size of 48 was calculated with 90% power and α error of 5%.
Results: DHA was significantly higher in term breast milk as compared to preterm breast milk (0.18 ± 0.08 ug % Vs 0.12 ± 0.09 ug % p = 0.025). The
levels of arachidonic acid and also overall PUFA were significantly higher in term milk. This difference was seen even though the dietary intake of fatty acids
in both groups was similar. Whether this has long term consequences needs to be investigated.
Conclusion: The levels of DHA was significantly lower among preterm infants’ mothers’ breast milk, compared to term infants, despite there being no
significant dietary differences between the two groups. Whether supplementation of DHA to pregnant women or preterm infants could improve neurological
and retinal outcomes is yet to be studied.
Keywords
DHA; Preterm; Breast milk; Fatty acid
Introduction
Docosahexaenoic acid (DHA) is an omega-3 fatty acid that is a
primary structural component of the human brain, cerebral cortex,
skin, and retina [1]. DHA comprises 40% of the polyunsaturated
fatty acids (PUFAs) in the brain and 60% of the PUFAs in the retina
[2]. The time of the most rapid neural and retinal development
occurs mainly during the third trimester (28-40 weeks of gestation).
Inadequacy of long chain n-3 fatty acids such as DHA during this
period can compromise brain function [3]. Preterm infants may be
disadvantaged by virtue of their shortened gestation and thereby
shortened transplacental transfer of these essential fatty acids (EFAs). Preterm neonates are also more likely to suffer complications
including cold stress and hypoglycemia. Even after recovering
from neonatal complications, they remain more prone to poor
physical growth and poor neurodevelopmental outcome [4]. Thus
early nutritional support of preterm infants is important because
it influences long-term health and development. Postpartum, the
major source of these EFAs is human breast milk, which is universally
considered as the optimal food for both term and preterm infants
[5]. It has been a matter of debate whether the fatty acid composition
of human milk differs in preterm as compared to term breast milk.
The breast milk content of LCPUFA is highly variable, depending on
geographic location, dietary habits and genetic influences. Brenna et al report a descriptive meta-analysis that included 65 studies of 2474
women. The highest DHA concentrations were primarily in coastal
populations and were associated with marine food consumption
[6]. This meta-analysis showed the variability of DHA worldwide.
However there is a dearth of studies quantifying the micronutrient
profile of the breast milk of Indian mothers. This study is designed
to compare the fatty acid composition in breast milk of Indian
mothers with preterm and full-term newborns and to determine the
relationships of dietary intake of docosahexaenoic acid (DHA) of
mothers and the content of this fatty acid in their milk.
Materials & Methods
Type of study: This observational, analytical study was conducted
in the postnatal wards and NICU of St. John’s Medical College
Hospital, Bangalore.
Subjects: Sample size (n=24 in each group) was calculated using
the Nmaster software to provide a power of 90% with an alpha error
of 5%. Institutional Ethical Review Board approval was obtained.
Samples were collected from mothers of 4-7 days old preterm (<37
completed weeks of gestation) and term neonates. The exclusion
criteria were multiple gestations, prior delivery less than 2 years from
the date of current delivery, diabetes in pregnancy, use steroids/
anticonvulsants or DHA supplementation during period of gestation
and maternal age less than 18 or greater than 40.
Sampling: The best gestational age of the neonate was calculated
by the first trimester ultrasound (T1 USG). In the absence of T1
USG, mothers were included only if the gestational age based on last
menstrual period and by Modified Ballard Score corroborated with
each other. The first group (n = 23) included mothers delivered at
term (gestational age from 37 to 42 weeks) and the second group (n
= 24) included mothers who delivered preterm i.e.,< 37 weeks. The
study was explained to the mothers and written consent was obtained
before sample collection. The mother’s age, parity, education status,
and eating habits were recorded. Body mass index was calculated
from prepregnancy weight / T1 weight (from the mother’s records)
and the mother’s height. The mothers also completed a food
record questionnaire (modified food frequency questionnaire)
to determine their food intake (during pregnancy). Total energy,
protein, carbohydrates and fatty acid composition were calculated
using nutrition software. Mothers expressed foremilk and hind milk
separately, and 2ml of hind milk was collected and stored for analysis.
The rest of the milk was used for feeding the baby. Milk samples were
stored at -700C till analysis.
Measurement of fatty acid status of breast milk: Fatty acids from
breast milk total lipids (from 500 μl of breast milk) were analyzed
using Gas chromatography with a flame ionization detector (Varian
3800; Varian, Palo Alto, CA, USA). Briefly, the procedure followed
involved the extraction of total lipids and trans-methylation of all fatty
acids from this fraction using BF3-methanol. 9 The fatty acid methyl
esters were then separated by chain length and degree of saturation by
injection onto a 50 m, 0.2 mm capillary column (FAME, Varian) with
nitrogen as carrier gas. Individual fatty acids were identified against
reference fatty acids.
The odd-chain FA - heptadecanoic acid, C17:0 was used as an
internal standard in each sample. Based on the internal standard, total
fatty acid contents of the samples were calculated and each identified
fatty acid was expressed as a percentage of the total content of the
identified fatty acids.
Statistical analysis: All analyses were performed using SPSS
Version 20. Difference between means was assessed by independent
samples t-test (DHA, other fatty acids). Correlation between
quantitative variables was tested by Pearson’s coefficient of correlation
(DHA & BMI/ maternal dietary DHA). P values less than 0.05 were
considered significant.
Results
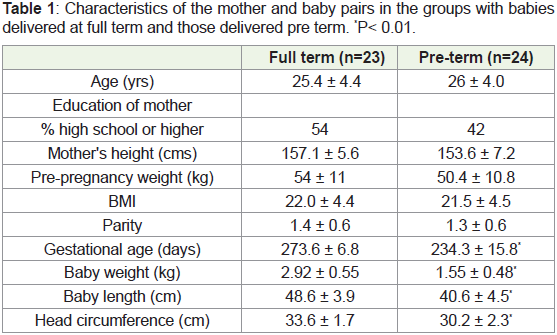
Table 1 gives the anthropometric and demographic details of the
women and their babies in both groups. No significant differences
were seen between the mothers in the two groups.
Table 1: Characteristics of the mother and baby pairs in the groups with babies
delivered at full term and those delivered pre term. *P< 0.01.
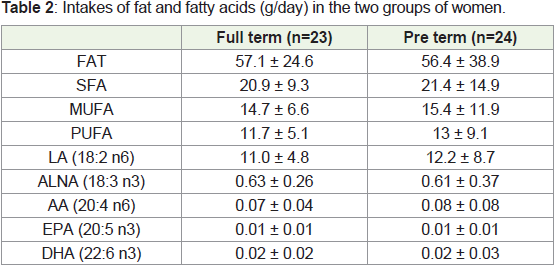
Table 2 provides the information on the fat intakes in the two
groups. No significant difference was seen in the dietary intakes of
the two groups of women. Intakes of LCPUFA were relatively low in
both groups.
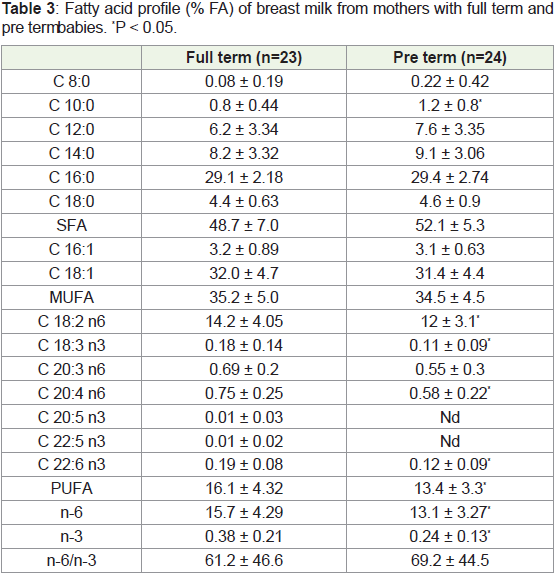
The fatty acid profile of breast milk is presented in Table 3. The
pre term milk was found to have relatively higher levels of SFA and
significantly lower levels of total PUFA as well as both n6 as well as
n3 PUFA. The n6/n3 ratio was seen to be high in both groups but not
statistically different between the groups.
Table 3: Fatty acid profile (% FA) of breast milk from mothers with full term and
pre term babies. *P < 0.05.
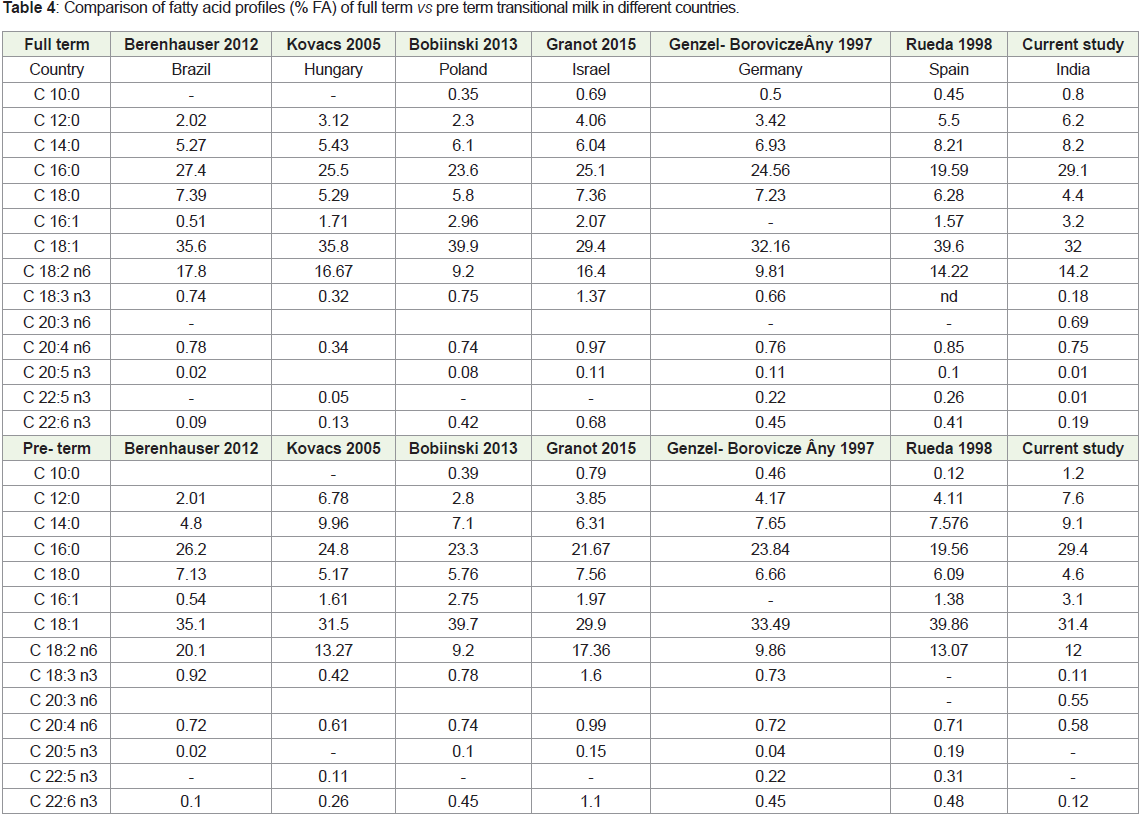
Table 4 provides a comparison of the fatty acid profile of full term
vs pre term transitional milk from various countries. A high degree of variability in composition is seen across these countries and the
results of the current study appear to be within these parameters.
Discussion
We enrolled mothers of 23 term and 24 preterm neonates. The
groups were similar with respect to maternal characteristics like age,
education, maternal height, pre-pregnancy BMI and parity.
Mothers in the preterm group had significantly lower levels of
breast milk PUFA. This is finding is similar to findings in the study
by Berenhauer et.al showing term mothers having a higher breast
milk PUFA content compared to preterm mothers and in contrast
to the study by Granot et.al showing no significant correlation [7,8].
Since there were no significant differences in the dietary PUFA
intake between the mothers from the term and preterm group, the
difference in PUFA levels in breast milk are likely to be attributed to
other factors, including genetic factors. Maternal age, height and pre
pregnancy weight were similar as well.
We also found that DHA in the breast milk of mothers of term
infants was higher in comparison to that of mothers of preterm
infants, despite there being no significant dietary differences between
the two groups. Kovac et al. found values of docosahexaenoic acid were significantly higher in human milk samples of mothers of
preterm as compared with full- term infants [9]. However Iranpour
et al found no significant difference in DHA in breast milk of preterm
and term mothers [10]. These contrasts could be attributed to the
period we have chosen for sample collection (we studied day 4-7
milk) and different sampling methods.
In our study, breast milk DHA levels on average for the entire
population (n=47) studied of 0.15±0.09. This was less than half of the
global average as reported in a descriptive meta- analysis by Brenna
et al [6]. The mean (+SD) concentration of DHA in breast milk (by
weight) was 0.32 + 0.22%. The highest DHA concentrations were
primarily in coastal populations and were associated with marine
food consumption. Notably there were no studies from India as part
of the review.
The mothers in our study consumed a predominantly vegetarian
diet. This possibly contributed to the low DHA levels found in their
breast milk. In a vegetarian diet, the DHA content is negligible.
Although the body can convert alpha - linoeic acid to DHA, the
maternal plasma levels produce lower concentrations of DHA in the
breast milk compared to meat eaters, especially those who consume
significant quantities of marine food.
However, a systematic review by Bravi et al. found only weak
correlation between diet and breast milk DHA levels, further
supporting the need for more systematic studies on this and the
role of other factors, including genetics, in determining DHA
levels of breastmilk [11]. A recent study by Sosa-Castillo et al. has
also emphasized the role of the interaction between maternal
diet and gene transcription mechanisms, resulting in variation in
the proportion of fatty acids in milk. These mechanisms, yet to be
completely elucidated, could explain the degree of variability in the
differing findings in studies trying to infer the relation of breast milk
composition with other variables.
The lower DHA levels in the breast milk of mothers are
disconcerting, as preterm infants by virtue of their shortened
gestation accumulate less DHA via transplacental transfer [12].
This is compounded by the fact a majority of that LCPUFA transfer
occurs during the third trimester and that the infant’s capacity to
produce DHA de novo is limited [13]. This may put preterm infants
at a disadvantage given the role DHA has been shown to have in the
development of neuronal tissue. Babies born preterm require higher
amounts of fatty acids than term babies for development. Few studies
have shown that supplementation of the same in the neonatal period
improves neuronal development. However, none of them were done
in India. The European Food Safety Authority (EFSA) recommends
100 mg per day as the adequate intake of DHA for children less
than 24 months of age [14]. However dearth of studies quantifying
the micronutrient profile of breast milk of Indian mothers makes it
difficult to objectively state whether the preterm infant is receiving
the advised intake. Larger epidemiological studies would be required
to assess breast milk fatty acid composition for the Indian population,
and the impact of omega 3 fatty acid supplementation on breast milk
composition. This is a promising area that could potentially improve the standard of care of preterm neonates, which could positively
influence long term neurological outcomes.
Conclusion
The levels of DHA were significantly lower among preterm
infants’ mothers’ breast milk, compared to term infants, despite
there being no significant dietary differences between the two groups.
Whether supplementation of DHA to pregnant women or preterm
infants could improve neurological and retinal outcomes is yet to be
studied. Also, mothers need to be educated about the importance of
fats in their diet and consequences of deficiency of PUFAs and DHA
in breast milk. In the long run, this would improve infant health and
neurological outcomes.
Limitations and scope for further studies
Our sample size was small and consisted of patients from only
one tertiary centre. This may not be representative of the entire
population and hence further studies are needed.
Even though the importance of DHA in neurological and retinal
development is known, more studies are needed to fully establish
the need to supplement DHA to newborns whose mother’s milk is
deficient and better outcomes.