Research Article
A Feasibility and Pilot Study in Nutrition Intervention for Child Health- Bangalore, India
Wong E1,2* and Shankar P2
1School of Public Health, Curtin University, Australia
2Red Element Health International, Singapore
Corresponding author: Wong E, School of Public Health, Curtin University, Perth, W.A., GPO Box U1987, Australia, E-mail: yee-sing.wong@postgrad.curtin.edu.au
Citation: Wong E, Shankar P. A Feasibility and Pilot Study in Nutrition Intervention for Child Health- Bangalore, India. Indian J Nutri. 2018;5(2): 192.
Copyright © 2018 Wong E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Nutrition | ISSN: 2395-2326 | Volume: 5, Issue: 2
Submission: 10/07/2018; Accepted: 03/08/2018; Published: 09/08/2018
Abstract
Indian schoolchildren residing in slum areas of Bangalore are at high risk of malnutrition thereby impairing their physical and mental development. These stunted and wasted schoolchildren of Parikrma Humanity Foundation may struggle to reach their full potential because of their poor nutritional status. Protein energy malnutrition is very common in these children due to insufficient protein and energy stores. Micronutrient deficiencies of iron, zinc, and vitamin A predominantly found in these children are known to affect their growth and cognition. Long-term malnutrition may lead to diet related disorders; increase morbidity and mortality; and kick-start a cycle of poor health and poverty. Malnutrition is a serious health problem affecting millions of children worldwide and the rates have been appalling in developing countries, especially in India. A feasibility and pilot study in nutrition intervention was implemented using convenience sampling in 2013 that aimed to explore perceptions and attitudes along with suggestions of students, doctors, parents, caterers, school staff and community development officers involved in the plan and structure of a full scale ‘Nutrition for Children’ program. This program conducted by the Singapore International Foundation volunteers was conducted in partnership with the Parikrma schools. Positive study outcomes justified an imperative need for continuation of a culturally appropriate community nutrition intervention to train all beneficiaries and key stakeholders to: understand key nutrition principles; impart culinary nutrient conservation skills; and act as positive role models to optimize the nutritional status of these schoolchildren. Valuable study insights and recommendations spurred the urgency for the volunteers to further plan, develop and evaluate a three-year (2014-2017) school-based nutrition intervention to build a more supportive environment for these malnourished children. By creating sustainable nutritional programs to motivate, empower and inspire the local community towards better healthy eating and hygiene practices, the malnutrition rates may be improved among schoolchildren.
Keywords:
Community-based; Health program; India; Malnutrition; Nutrition education; Schoolchildren
Abbreviations
CDO: Community Development Officers; GHI: Global Hunger Index; ICDS: Integrated Child Development Scheme; MDMS: Midday Meal Scheme; NGO: Non-Government Organizations; PHF: Parikrma Humanity Foundation; PEM: Protein-Energy Malnutrition; SIF: Singapore International Foundation; VAD: Vitamin A Deficiency
Introduction
Impact of malnutrition in children
Children need healthy food for their growth and survival. Food provides them with the energy to carry on their daily activities. However, poor nutritional status in children can lead to a condition termed as malnutrition that encompasses ‘undernutrition’ [1]. Undernutrition occurs when their diet provides them with insufficient nutrients needed for their overall development [2]. It includes stunting- when the child shows low height for his age; and wasting- when the child has low weight for his age [3]. Stunted and wasted children are unable to reach their full potential due to their nutritional deficiencies. Protein- Energy Malnutrition (PEM) is a form of malnutrition which occurs due to insufficient protein and energy stores, clinically classified into three types: marasmus (wasting from malnutrition), kwashiorkor; and marasmic kwashiorkor [4]. PEM weakens a child’s immune system, affecting their ability to fight the common cold and flu and extending their duration of illness [4]. In the long term, impairment of their physical and mental development can have adverse effects on their academic performance in schools [5].
When a child is malnourished, it also gives rise to several other micronutrient deficiencies, affecting the functional performance of these children [6]. Major deficiencies such as iron, zinc, vitamin A, and iodine are of utmost significance to public health in Asian children [1]. Among them, iron deficiency anemia seems to be of major concern since it affects more than 90% of children living in poor Indian households [7]. Furthermore, it causes developmental disorders that affect their cognitive capabilities such as poor attention span, memory, concentration and concept acquisition [7]. Recent evidence has also emphasized the importance of zinc in the growth and development of children as its deficiency has been identified as a crucial factor in restricting child growth in developing countries [8]. Vitamin A Deficiency (VAD) is known to affect around 2.8 million preschool children in over 60 countries [8]. Morbidity and mortality risks are highly associated in children with severe and marginal cases of VAD, and stunting is reported in those who exhibited clinical symptoms of VAD [8].
Rationale for nutrition intervention in India
Malnutrition is a serious public health problem that affects millions of children in underdeveloped countries [9]. In fact, 80% of these undernourished children live in just 20 countries that broadly comprise of Africa, Middle East, Asia and the Western Pacific [1]. However, what has been more appalling is that malnutrition rates are especially prominent among Indian children under the age of five years [10]. According to the 2016 Global Hunger Index (GHI) Report, India was ranked 97th among all the 119 developing countries but increased in ranking to 100th in 2017 where its high GHI score was calculated based on various parameters i.e. undernourishment, child wasting, stunting and mortality [11,12]. The United Nations Children’s Education Fund in 2012 reported that nearly 31% of stunted and 42% of underweight children among all developing countries belong to India [13]. It was found that children residing in urban slums were poorest and fared worst in nutritional anthropometry; and had the highest rates of vitamin and micronutrient deficiencies in comparison to the urban and rural average. Malnutrition was evident in children living in poor households lacking basic resources to support life [14]. These children are more likely to suffer from the consequences of malnutrition, later on in their life, leading to early death [15]. Therefore, there is a compelling need to conduct a feasibility and pilot study in nutrition intervention in India to identify appropriate strategies to reduce incidence of malnutrition in schoolchildren.
Limited nutrition research in India
Malnutrition among children is of a growing concern, specifically in India as this condition has been increasing at an alarming rate as compared to other developing countries [16]. Research showed a significant improvement in mother’s feeding practices and the infants thrived after mothers were given nutrition education for a year [17]. This study displayed that nutrition interventions targeted towards parents as primary caregivers can have a positive impact on the health of their children and can play a crucial role to prevent and control malnutrition if they are consistent in their efforts [17]. As women play a huge role in food selection, preparation and distribution, a six-month horticulture nutrition education program targeted towards impoverished women was conducted in Tirupathi, India to provide them with the necessary skills in developing their own kitchen garden [18]. The nutrition program encouraged them to consume home-grown fruits and vegetables that were inadequate in their diets and involved weekly lectures; discussions and skits; and interactions with the beneficiaries [18]. Their nutritional knowledge was accessed before and after the program. Results revealed an optimistic increase in nutritional knowledge on fruits and vegetables and demonstrated improvements in dietary intakes of energy, protein, fat, vitamin A, thiamin, riboflavin, ascorbic acid, calcium and iron in the participating families [18].
Challenges of government initiatives on nutrition
In India, malnutrition has received attention from the government. Initiatives and policies have been implemented to tackle this problem. Currently, two large scale nutrition intervention programs are in place to address malnutrition across all states of India. The Integrated Child Development Scheme (ICDS) and Midday Meal Scheme (MDMS) are the two programs targeted towards improving the nutritional status of these children [19]. The ICDS scheme has been in effect since 1975 and is the largest nutrition intervention program running in India aim to improve the health and development of children below six years old [20]. This program was initially operated in only 33 village administrative blocks but was implemented all across India by 2007 [20]. Some ICDS programs include preschool education; immunization; growth monitoring; pre and post-natal care; nutrition education; life skills training for girls in their adolescent years; supplemental food programs; and distribution of fortified foods and micronutrient supplements [21]. These services are managed by trained Anganwadi community health workers and are offered at both the household level and in Anganwadi centers [21]. Major challenges include: providing frequent in-service training for these workers; huge population size; great diversity across India; lack of funding; absence of community awareness; which hinders effective scaling up of these programs for improving child development and well-being [20]. Moreover, implementation quality is also affected by the low institutional capacity and poor infrastructure [20]. The MDMS initiated in Tamil Nadu in 1995 had the objective of increasing the number of students attending government-aided schools at the primary level as well as to improve their nutritional status [19]. In 1997-2009, the scheme was implemented nation-wide and covered all primary school levels [19]. Every schoolchild is entitled to freshlycooked hot meals, believed to help improve academic performance [19]. However, a major drawback is that the hot meals served to these children focused only on meeting caloric requirements but were nutritionally inadequate and did not meet their daily requirement for protein, vitamins and minerals [19].
Other nutrition initiatives in Bangalore
In Bangalore, some philanthropic and Non-Government Organizations (NGOs) have been working hard to support the government in fighting hunger among schoolchildren [22]. NGOs such as The Sri Sai Mandali Trust at Malleswaram, Bangalore have been providing free mid-day meals to children in governmentaided schools [22]. The Sri Sai Mandali trust sponsored mid-day meals on a weekly basis to 41 schools (25 rural and 16 urban) that were part of a cross-sectional study that conducted anthropometric measurements i.e. height for age and weight for age to assess the nutritional status of these children [22]. This study highlighted the importance of a mid-day meal program as the nutritional status of these schoolchildren improved significantly [22]. Evidence has suggested a positive relationship between nutritional status indicators such as stunting, wasting, and under nutrition with poor academic performance in schoolchildren [15]. Based on our preliminary observations, we noticed limited nutrition intervention studies were conducted to assess malnutrition in schoolchildren residing in Bangalore slums. Hence, this feasibility and pilot study on nutrition intervention program is imperative to justify the development of a full-scale nutrition program for these malnourished schoolchildren. Parikrma Humanity Foundation (PHF) was primarily selected as an appropriate intervention site for this intervention as PHF has prior working partnerships with the Singapore International Foundation (SIF) and nutrition was a key priority raised by various parents and Community Development Officers (CDO) through informal school meetings and internal observations.
Methods
A feasibility and pilot study was designed and implemented from 2013-2014 at PHF that runs four schools (Sahakarnagar, Jayanagar, Nandini and Koramangala) for 1500 schoolchildren between the ages of 5 and 17 years, belonging to 69 slum communities and 4 orphanages across Bangalore. Verbal and written informed consent for inclusion in the program and to being interviewed and tape recorded were obtained from the founder, teaching staff of PHF, all parents, caterers and doctors prior to program commencement. After the initial invitation by CDOs, eligible participants were informed of their rights and confidentiality issues, and that they were free to withdraw at any stage. Participants volunteered to be in the program were not identified in any transcription and all personal information was kept strictly confidential. All participants submitted their informed consent before their participation in the program. The program was conducted in accordance with the principles elucidated in the Declaration of Helsinki.
Feasibility study
Prior to the pilot study, assessment on feasibility of the nutrition program was done by consolidating information and data collected from 1) anthropometric assessment; 2) feasibility questionnaire; and 3) site visit; as described in the following sections:
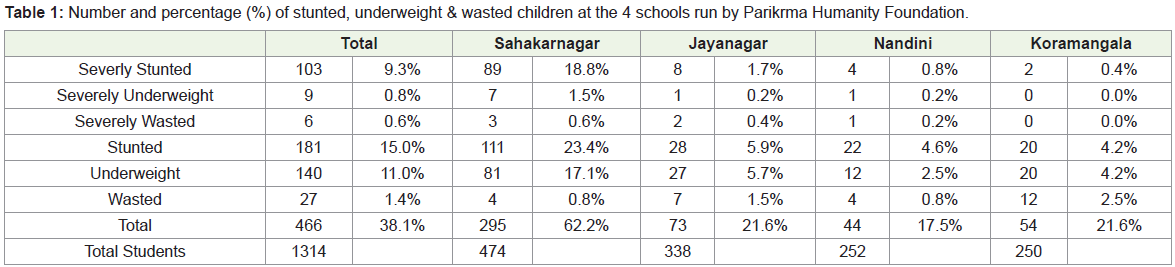
Anthropometric assessment: Anthropometric assessments were conducted by all CDOs and teaching staff over a period of one month on all schoolchildren aged 5-17 years attending the four schools under PHF to assess the number and prevalence of severely stunted, underweight & wasted schoolchildren versus stunted, underweight & wasted schoolchildren (Table 1).
Data categorization using stature-for-age and weight-for age percentile charts for girls (Supplementary file 1) and boys (Supplementary file 2) aged 2-18 years were necessary to categorise those schoolchildren as severely malnourished. These school children were given a higher priority for addressing their nutritional needs and concerns by the CDOs. Height was measured with measuring tapes attached to the walls and weight was measured using calibrated weighing machines provided in the principals’ offices across the 4 schools.
Feasibility questionnaire: Two SIF volunteers, in collaboration with the PHF staff fully in charge of this project, planned a feasibility study in 2013 to examine nutritional knowledge, attitudes, concerns, issues and needs of all beneficiaries and stakeholders involved in the children’s health and well-being. The questionnaire to assess the feasibility for this nutrition program (Supplementary file 3) was developed, pilot tested and implemented by the CDOs and SIF volunteers over a period of 2 weeks. Face-to-face interviews of approximately 30 minutes each were performed on the beneficiaries and stakeholders: students, medical doctors, parents, caterers, teachers, CDOs and principals from each of the 4 schools using convenience sampling. Data collected was essential to inform suitable content materials, outline and topics for the creation of a “Nutrition for Children” program to address malnutrition among these schoolchildren.
Site visit: Various site visits were made by SIF volunteers and PHF staff to the school compounds of PHF, medical clinics, residential slums of severely malnourished schoolchildren, and food catering venues. Nutritional analysis was conducted on the cyclic catered menus provided by the food caterers to the schools. Photo taking (See Supplementary file 10: Schoolchildren having their lunch meals; and Supplementary file 11: Home visits), video recording, note taking and field trip observations were implemented at all these sites to generate reports. Documentation of such information was useful to inspect physical, social and economical barriers and motivators in the development of a culturally relevant nutrition program.
Pilot program
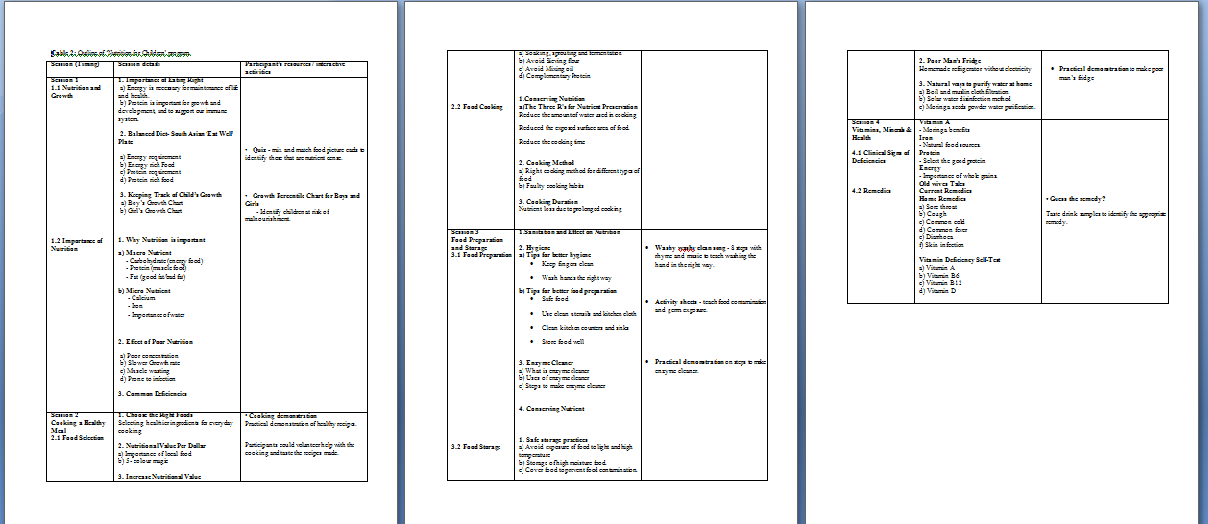
Six months after the feasibility study, the ‘Nutrition for Children’ program outline (Table 2), nutrition community project plan (Supplementary file 4) and trainer’s manual (Supplementary file 5) were developed and implemented by the SIF volunteers with the support of local dietitians to empower parents, teachers, and CDOs by educating them on the following key messages:
Convenience sampling was employed to recruit parents, food caterers, teachers, principals and CDOs to attend the program through invitation by staff of PHF. This 2-week school based nutritional training program was aimed to provide 1) parents with hands-on culinary skills, knowledge on preparing nutritionally balanced meals and the importance of food hygiene; 2) caterers and principals on the importance of nutritious meals for child growth; and 3) CDOs and teaching staff with nutritional knowledge and skills to train other beneficiaries and act as health advocates to drive healthy eating and hygienic practices. After attending the program, reinforcement tools on healthy practices such as an Aloe Vera plant, reusable food containers and nail clippers were given to all participants.
Results
Feasibility study
Findings reported high prevalence of malnutrition across all schools, but the highest rate was found among schoolchildren residing in Sahakarnagar slums. The anthropometric measurements at Sahakarnagar indicated that: 200 (42%) schoolchildren were stunted and severely stunted; 88 (18.6%) were underweight and severely underweight; and 7 (1.4%) were wasted and severely wasted. This was followed by Jayanagar; where 36 (8%) schoolchildren were stunted and severely stunted; 28 (6%) were underweight and severely underweight; and 9 (2%) were wasted and severely wasted. At Koramangala, 22 (5%) schoolchildren were stunted and severely stunted; 20 (4%) were underweight and severely underweight; and 12 (3%) were wasted and severely wasted. Lowest prevalence rate was found at Nandini; where 26 (5%) schoolchildren were stunted and severely stunted schoolchildren; 13 (3%) were underweight and severely underweight; and 5 (1%) were wasted and severely wasted.
Data collected from the interviews and site visit observations revealed the following main findings:
- Addition of small portion of brown rice/parboiled rice to the regular white rice.
- Addition of soya flour to wheat flour to increase the protein content of the chapatti.
- Supplementing meals with different lentils or adding soya meal maker/soya chunks to increase the protein content.
- Adding more mixed vegetables and the inclusion of five colours to add more variety and nutrients.
- Using more local vegetables to reduce cost.
- Including nuts like peanuts that are easily available and affordable to increase calories, healthy fats and proteins.
These findings based on data collected were incorporated into the training manual aimed to make a positive difference in the health status of the schoolchildren, their families and local communities.
Pilot program
After the completion of the feasibility study, a piloted nutrition education program was developed, implemented, and evaluated. Feedback was obtained from participants and it was observed that they scored moderately high in using new skills from the program: 1) recalling information learnt at the pilot study program (89%); 2) describing what they had learnt to a colleague or family member (92%); 3) applying what they had learnt to solve health problems at home or work (80%); 4) applying what they had learnt to achieve health improvements (80%); and 5) applying what they had learnt to experience positive changes in their local community (82%). Major skills that they learnt and enjoyed most during the workshops related to the preparation of the fruit peel enzyme cleanser; healthier cooking methods; food hygiene practices; and home remedies. Parents’ feedbacks were encouraging as they mentioned that they could apply these new learnings to a higher level by starting their own business in making enzyme cleansers that could impact upon and enhance their own livelihood. Some valuable quotes that reflected their appreciation for the pilot program are as follows:
“What we learnt and experienced today, I am not going to pack this and put it away. I am going to use this to benefit the community” Shanta, Mother of 2
“I think this programme went on extremely well because it was well thought-out, well-planned & culturally-sensitive. It was comprehensive & done in a humble & friendly manner for our participants. We know that they will be carrying this message back into their community, so the spread is going to be even wider.” Shukla Bose, PHF Founder.
Discussion
The feasibility study confirmed a high prevalence of malnutrition; inadequate nutrients in catered school meals; poor nutritional knowledge, skills and hygienic practices among PHF schoolchildren and their beneficiaries especially in Sahakarnagar districts. Therefore, a pilot study was developed, implemented and evaluated to improve upon the implementation of a full-scale “Nutrition for Children” program. This program aimed to enhance the nutritional status of malnourished children residing in Indian slum communities. It focused on educating all stakeholders & beneficiaries on nutrition for growth; food preparation and storage within their limited budget; nutrient deficiencies and home remedies to ensure healthier diets for their families and local community. It also assessed appropriateness and suitability of program materials, activities and resources.
Positive feedback was given by all beneficiaries and stakeholders who were happy and grateful to the SIF volunteers for conducting the workshops for PHF. Teaching staff and principals appeared to be confident in delivering these nutrition messages after attending the program and developed an excellent rapport with the parents, together with the support of the CDOs which is important in encouraging all parents and caterers to implement these ideas and teachings into community action.
Media coverage of the pilot run of the “Nutrition for Children” in Bangalore, India was posted on the SIF website [23]; “Happy and Healthy: Nutrition for the Parikrma Soul” [24]; ( Supplementary file 12) and “Eating for a Healthier Tomorrow” (Supplementary file 13) articles were published in PHF newsletters [25]. Results from this feasibility and pilot program further drove the continuation of a comprehensive 3-year nutrition intervention from 2014 - 2017 that benefitted more than 1,500 children (from marginalized families), 1,200 families with estimated outreach to a total of 6,000 beneficiaries. This program has also kick-started an interest in PHF teachers to develop fun, practical teaching activities to reinforce nutritional messages and implement them in their students’ educational curriculum and framework. If these students apply these messages as part of their early life practices, it may provide them lifelong benefits for their future generations within the Indian society.
Major challenges experienced by the SIF volunteers were 1) language barriers; 2) lack of manpower; and 3) monitoring of health practices among participants. Majority of the participants spoke in Kannada and the SIF volunteers spoke mainly in English or Hindi. CDOs and teaching staffs volunteered to serve as translators. However, SIF volunteers were uncertain if all nutritional messages were accurately and effectively conveyed to the participants. Thus, local dietitians were engaged in the pilot program to minimize any inaccuracy in knowledge translation. Locum dietitians and community nutritionists could be taught by the SIF volunteers to conduct future training to mobilize more manpower resources. Prior arrangement with the local hospitals or government organizations to encourage future training of dietetics or health promotion students as part of their locum training hours can be fulfilled through provision of community internships at PHF to assist in the ‘Nutrition for Children’ program. Their nutritional background and expertise could assist in designing more culturally appropriate teaching resources or in the development of other nutritional topics that is beneficial to the nutritional status of school children. After training the CDOs, their roles are to conduct site visits: to monitor eating practices of students; enforce healthier cooking methods and maintenance of hygiene practices by parents; and the observation of healthier meals prepared by the school caterers. Together with teaching staff within the PHF vicinities, they are to act as health ambassadors to promote healthy eating practices and ensure that incidence of malnutrition is reduced among the schoolchildren. The continual support and active engagement of parents, caterers, teaching staff, and CDOs in this program are paramount to improve the nutritional status of Indian schoolchildren that may impact their learning performance. This ‘Nutrition for Children’ program spearheaded by the SIF volunteers will create sustainable nutritional improvements to live healthier lifestyles through a reciprocal effect for the schoolchildren, their families and communities not only within PHF vicinities, but can also be generalized to other regions within India.
Conclusion
Nutrition school education can play a vital role in mitigating malnutrition rates among schoolchildren. Both the feasibility and pilot program provided a baseline for improving its program implementation. It gave opportunities to identify suggestions, feedback and challenges in program implementation. By incorporating all these findings to promote optimal nutritional practices, all CDOs and teaching staff of PHF together with the support of SIF volunteers will be better equipped to nudge participants such as parents and caterers in their pursuit to enhance the schoolchildren’s nutritional status within their local districts.
Acknowledgements
The authors are grateful to Singapore International Foundation, Red Element Health International, the founder, principals, teachers, and CDOs of PHF; caterers; and medical doctors involved in the feasibility and pilot study for their kind support and contribution to the study. We are also thankful to all the Indian parents who have participated in the intervention.
References
- Ahmed T, Mahfuz M, Ireen S, Ahmed AM, Rahman S, et al. (2012) Nutrition of children and women in Bangladesh: trends and directions for the future. J Health Popul Nutr 30: 1-11.
- Bagilkar VV, Savadatti BB (2015) A descriptive study on Malnutrition. Asian J Nurs Educ Res 5: 72-77.
- Peterson K (2009) Viewpoint: childhood undernutrition: a failing global priority. J Public Health Policy 30: 455-464.
- Faruque AS, Ahmed AM, Ahmed T, Islam MM, Hossain MI, et al. (2008) Nutrition: basis for healthy children and mothers in Bangladesh. J Health Popul Nutr 26: 325-339.
- Grantham-McGregor S (1995) A review of studies of the effect of severe malnutrition on mental development. J Nutr 125: 2233S-2238S.
- Swaminathan S, Edward BS, Kurpad AV (2013) Micronutrient deficiency and cognitive and physical performance in Indian children. Eur J Clin Nutr 67: 467-474.
- Haldar D, Chatterjee T, Sarkar AP, Das SK, Mallik S (2011) A Study on the role of parental involvement in control of nutritional anemia among children of free primary schools in a rural area of West Bengal. Indian J Public Health 55: 332-335.
- Bhutta ZA, Salam RA, Das JK (2013) Meeting the challenges of micronutrient malnutrition in the developing world. Br Med Bull 106: 7-17.
- Nahar B, Hamadani JD, Ahmed T, Tofail F, Rahman A, et al. (2009) Effects of psychosocial stimulation on growth and development of severely malnourished children in a nutrition unit in Bangladesh. Eur J Clin Nutr 63: 725-731.
- World Bank (2013) Helping India combat persistently high rates of malnutrition.
- Mishra CP (2017) Malnutrition-free India: Dream or reality. Indian J Public Health 61: 155-162.
- Grebmer KV, Bernstein J, Brown T, Prasai N, Yohannes Y, et al. (2017) Global Hunger Index - The Inequalities of Hunger.
- Sankar R, Van den Briel T (2014) Prospects for better nutrition in India. Asia Pac J Clin Nutr 23: S1-S3.
- Ghosh S, Shah D (2004) Nutritional problems in urban slum children. Indian Pediatr 41: 682-696.
- Rashmi MR, Shweta BM, Fathima FN, Agrawal T, Shah M, et al. (2015) Prevalence of malnutrition and relationship with scholastic performance among primary and secondary school children in two select private schools in Bangalore Rural District (India). Indian J Community Med 40: 97-102.
- Burtscher D, Burza S (2015) Health-seeking behaviour and community perceptions of childhood undernutrition and a Community Management of Acute Malnutrition (CMAM) programme in rural Bihar, India: a qualitative study. Public Health Nutr 18: 3234-3243.
- Guldan GS, Fan HC, Ma X, Ni ZZ, Xiang X, et al. (2000) Culturally appropriate nutrition education improves infant feeding and growth in rural Sichuan, China. J Nutr 130: 1204-1211.
- Sarada D, Rajani N (2012) Horticultural nutrition intervention through women’s participation: An action research. J Human Eco 38: 71-80.
- Arumugam A (2016) Understanding school feeding programmes in India and Tamil Nadu in addressing classroom hunger. Int J Educ Multi Stu 4: 116-125.
- Rao N, Kaul V (2018) India’s integrated child development services scheme: challenges for scaling up. Child Care Health Dev 44: 31-40.
- Ramakrishnan U, Lowe A, Vir S, Kumar S, Mohanraj R, et al. (2012) Public health interventions, barriers, and opportunities for improving maternal nutrition in India. Food Nutr Bull 33: S71-S92.
- Shalini CN, Murthy NS, Shalini S, Dinesh R, Shivaraj NS, et al. (2014) Comparison of nutritional status of rural and urban school students receiving midday meals in schools of Bengaluru, India: a cross sectional study. J Postgrad Med 60: 118-122.
- Ng E (2014) Pilot run of IV project nutrition for children in Bangalore, India.
- Parikrma Humanity Foundation (2014) Parikrma Humanity Foundation Newsletter. Happy and Healthy: Nutrition for Parikrma Soul.
- Parikrma Humanity Foundation (2014) Parikrma Humanity Foundation Newsletter. Eating for a Healthier Tomorrow.