Research Article
MRI Scanning in Young Children: Child- Focused Play Intervention Reduces Sedation and Improves Parental Satisfaction
P Pramod Kumar1, Bhavneet Bharti2, Prahbhjot Malhi2* and Akshay Kumar Saxena3
1Department of Pediatrics, Government General Hospital, Wanaparthy, Telangana. India
2Department of Pediatrics, Post Graduate Institute of Medical Education and Research, Sector 12, Chandigarh 160012. India
3Department of Radiodiagnosis and Imaging, Post Graduate Institute of Medical Education and Research, Sector 12,
Chandigarh – 160012. India
*Corresponding author: Prahbhjot Malhi (Professor, Child Psychology), Department of Pediatrics, Post Graduate Institute
of Medical Education and Research, Sector 12, Chandigarh – 160012. India Email: pmalhi18@hotmail.com
Copyright: © 2023 Pramod Kumar P, et al. This is an open access article distributed under the Creative Commons
Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original
work is properly cited.
Article Information: Submission: 14/09/2021; Accepted: 16/01/2023; Published: 19/01/2023
Abstract
Objective: To examine the impact of a non-invasive strategy, such as a customized play activity, in reducing the need for sedation in young children
undergoing diagnostic magnetic resonance imaging (MRI).
Methodology: A randomized controlled trial design was used. All children (4-7 yrs) undergoing diagnostic MRI at the department of paediatrics of a
tertiary care hospital were eligible for enrolment. The exclusion criteria included history of development delay, previous MRI scan, and acute traumatic or
painful condition. A total of 164 children (83 in control and 81 in intervention arm) were recruited. The intervention involved familiarization with MRI procedure
and scanner using a mock scanner, training the child to stay motion free in the machine, and providing the child multiple trial-runs of the MRI imaging with
a favoured toy.
Results: The two groups of children were matched on age, gender, and education level of the mother. The percentage of children receiving sedation
in the intervention group was 49.4% and this was lower than the control group (63.8%), however, the difference did not approach statistical significance
(χ²=3.5, P=0.06). Comparison of the groups on the secondary outcome measure of ease of performing scan by the ratings of a radiologist, blinded to group
status, revealed that a significantly higher proportion of the intervention group scans were reported to be easy or extremely easy, relative to the control group
(χ²=10.83, P= 0.013).
Conclusion: The study underscores the need for using a child-centric approach in diagnostic testing as this considerably improves family satisfaction
and reduces need for sedation.
Keywords
MRI; Child-Focused Play Intervention; Sedation, Parental Satisfaction
Introduction
Magnetic resonance imaging (MRI) is a commonly used
procedure in children to get the structural details of the organs. The
procedure itself is painless and non-invasive but the MRI scanner environment for children is anxiety-provoking. The scanning
procedure requires children to remain motionless for a prolonged
duration of time in an enclosed and unfamiliar equipment, be
exposed to loud noises, and sometimes also involves needle insertion
for intravenous administration of contrast agents [1]. The distress children experience during the procedure can lead to restlessness,
excessive crying, and refusals contributing to poor quality imaging
and delays in diagnosis and treatment. Excessive distress can also
have a profound effect on the physical and psychological well-being
of children [2]. In order to circumvent some of these adverse effects,
the current clinical practice uses sedation in children to guarantee
good quality MRI scans. Some of the associated medical risks of
sedation include cardio- respiratory depression, airway obstruction,
motor imbalance, hypoxia, and hypotension [3]. Since anaesthesia is
detrimental to the child’s safety, several ethical concerns for its use in
diagnostic testing have been raised [4].
Several behavioral interventions have been developed to reduce
head motions during neuro-imaging sessions, increase relaxation,
and promote procedural understanding as alternatives to sedation
among children [5]. Some of these interventions include the creation
of a child and family-friendly MRI environment [6], use of play and
guided imagery [7], mock scanner training educational training
using toy scanners, videos, play tunnels, and audio simulations
[8], virtual reality [9], video-based education [10], relaxation and
distraction techniques [11], and psychological interventions (clown
shows, music, pets) [12]. All these interventions have been reported
to be advantageous in reducing anxiety before and during an MRI
procedure.
Using child-friendly techniques to reduce distress before medical
procedures and surgery is routinely used in the West; however, their
use in India is relatively recent. Indeed, in India, clinicians spend
little time for preparing children or their families for the radiological
investigations. Some of the reasons cited include constraints of time,
an excessive rush of patients, and lack of awareness of alternative
techniques. One drawback of the research on alternatives to sedation
among children is that most studies have focused on older patients.
The present study redresses this imbalance by extending previous
literature on a much larger sample of younger children using a wider
range of outcome measures. Specifically, the present study aimed to
study the impact of an MRI customized play activity on the need for
sedation in young children aged 4-7 years undergoing diagnostic
MRI using a randomized control trial study design.
Methodology
The study was designed as a prospective randomized controlled
trial and all children undergoing Diagnostic MRI at the department
of pediatrics of a tertiary care hospital in the age group of 4 to 7
were eligible for enrolment. The exclusion criteria included a history
of development delay, previous MRI scan, and acute traumatic or
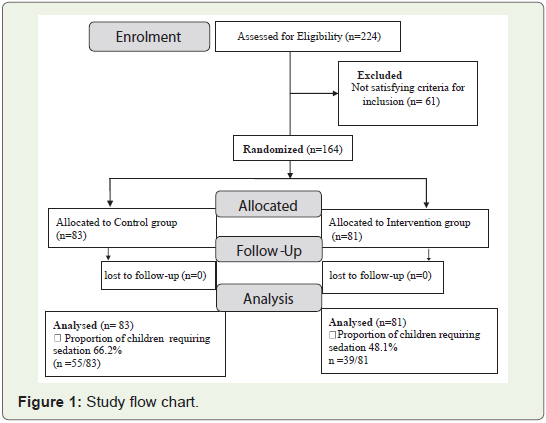
painful condition. A total of 164 children (83 in the control arm and
81 in the intervention condition) were recruited. The flow chart of the
study is presented in Figure 1. Group allocations were done based on
computer-generated varying block randomization procedure wherein
allocations were sequentially numbered and hidden in opaque sealed
envelopes. Written informed consent was obtained from parents
before randomization and ethical approval was obtained by the
Institute’s ethics committee.
Sample Size Calculation: The size of the sample was calculated
assuming the fraction requiring sedation in the control group as 40% and the ability to bring an absolute reduction of 20% in the
intervention group, with the power of 80% and an alpha error of 5%.
These assumptions were based on our previous research study.
Procedure: The detailed MRI customized play activity
intervention used in the present study has been standardized and
described in our previous study [7]. Briefly, the intervention involved
three phases of training. In the first phase of the training, children
were familiarized with the procedure and the MRI scanner using a
mock scanner machine. During this phase, the child was repeatedly
exposed to the loud acoustic noise in the scanner. The child was also
asked to select his/her favorite doll/toy and this was placed in the MRI
model and the child was allowed free play. In the second phase, the
child was trained to stay motion free in the machine by playing games
like ‘turning to stone.’ In the final phase of the training, the child was
asked to carry out multiple trial-runs of the MRI imaging with the
favorite doll/toy. On the day of the imaging, one of the training team
members accompanied the child and the parent/caregiver for the
procedure. Twenty minutes was allowed before imaging, and in case
the radiologist, who was blinded to the study, felt that the child would
not cooperate during the MRI procedure, the child was sedated as per
the standard protocol.
The primary outcome measure was the percentage of children
requiring sedation by group status. In addition, two secondary
outcomes were selected. The first was the ease of conducting the
procedure rating by the radiologist, who was masked to the group
allocation, on a 4-point Likert scale ranging from very difficult to very
easy. The second secondary outcome was the rating of the parent/
caregiver on the satisfaction with the procedure (dissatisfied or
satisfied).
Results
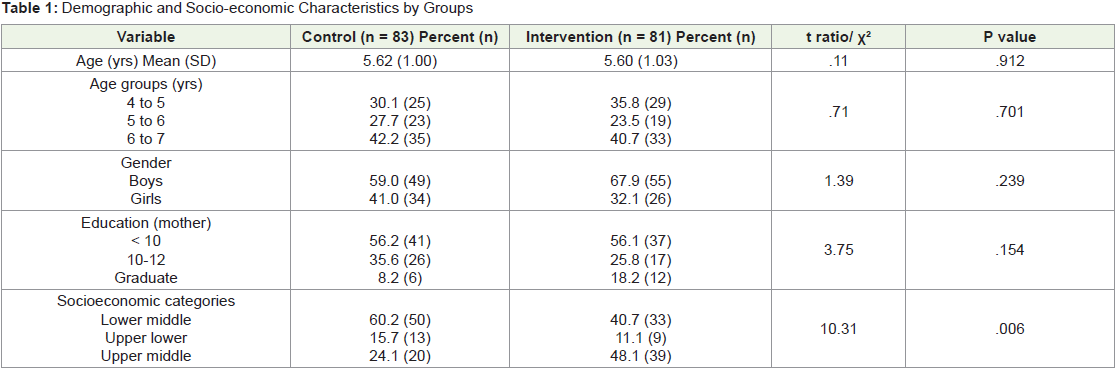
The mean age of the sample was 5.61 years (SD=1.01) and the study
population was primarily from urban areas (81%). The randomized
intervention and control groups were well matched and did not differ
on age (t=.11, P=0.701) and gender of the child (χ²=1.39, P=0.239),
and education level of the mother (χ²=3.75, P=0.154.) However,
nearly twice as many children from the upper socio-economic status group in the intervention group as compared to the control group
(χ²=10.31, P= 0.006) (Table 1).
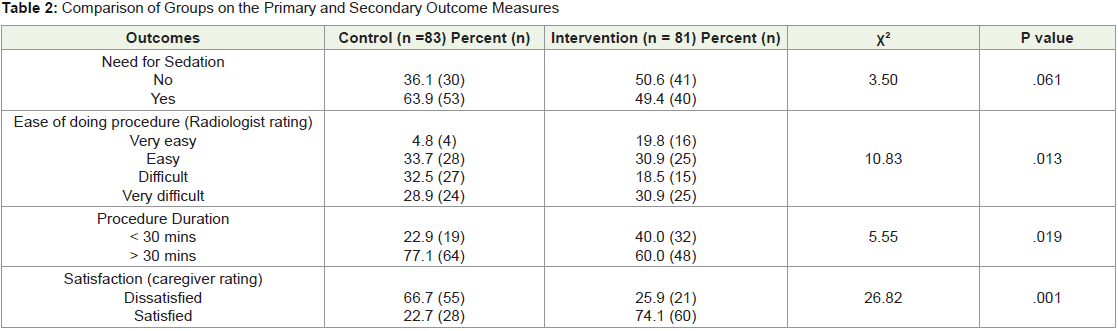
Table 2 presents the comparison of the two groups on primary and
secondary outcomes. The percentage of children receiving sedation in
the intervention group was 49.4% and this was lower than the percent
receiving sedation in the control group (63.8%). The absolute risk
difference in being sedated during the MRI procedure was 14.4%
lower in the intervention group (with 95% CI of 29.5% lower to 0.5%
higher risk in the intervention group). The risk ratio (RR) of receiving
sedation during MRI was 23% lower in the intervention relative to
the control group (RR 0.77, 95% CI: 0.59-1.02; P= 0.06). Although
more than half (56%) of the children in the intervention group did
not require any sedation during MRI scan as compared to a lower
proportion of control subjects, the difference showed a trend although
it did not approach statistical significance (χ²=3.50, P= 0.061).
Comparison of the groups on the secondary outcome measure
of ease of performing scan by the ratings of a radiologist, blinded to
the group status, revealed that a significantly higher proportion of
the intervention group scans were reported to be easy or extremely
easy, relative to the control group (χ²=10.83, P= 0.013). In fact,
the relative risk of an MRI being reported as “very easy” increased
by 1.77 times in the intervention as compared to the control group
(RR 1.77; 95% CI: 1.33-2.35) and this effect size was significant (P=
0.0035). In addition, a higher percentage of the parents of children
in the intervention group (74.1%) were satisfied with the procedure as compared to a much lower percentage of parents from the control
group (22.7%) (χ²=26.82, P=0.001). The risk of parents reporting as
‘not satisfied’ with the MRI procedure decreased by nearly 60% in
children who underwent the play-based intervention as compared to
the control group (RR 0.39; 95% CI: 0.26-0.58) and this result was
also significant (P=0.001). These results demonstrate that play-based
intervention was useful in reducing the dose of sedatives and parental
dissatisfaction with the procedure.
Discussion
The primary objective of the study was to examine the impact of a
non-invasive strategy, such as a customized play activity, in reducing
the need for sedation in young children (4-7 yrs) undergoing
diagnostic MRI, using a randomized control trial study design. The
findings indicate that the use of a play-based technique substantially
reduced the need for general anesthesia relative to controls.
These results extend previous findings and add to the literature by
demonstrating that young children too can benefit significantly from
a play-based structured intervention in the Indian setting. Previous
studies have documented the positive benefits of interventions
with older children [7,13] and demonstration of effectiveness in
young cognitively immature children is limited, especially in low resource
settings. The combination of the MRI scanner model and
play activity intervention is a cost-effective, safe, engaging, and fun
way to reduce the frequency of sedation in young children. There are
several other advantages as well such as increase in consumer safety,
parental satisfaction, easing the flow of patients in the radiologic units, and substantially lowering the burden of management during
the procedure. Notably, for younger children, the benefits of learning
from a live three-dimensional demonstration far exceed the benefits
of viewing it on a two-dimensional video screen [14-15].
Previous studies conducted in the developing countries have
demonstrated the use of play- based techniques with younger children
and with children with neurodevelopmental disorders. For example,
in a retrospective audit study, Carter et al found that the need for
general anesthesia in the mock MRI group was 17% lower relative
to the non-mock MRI group for 3 to 8 yr olds [16]. Barnea-Goraly
et al in a multi-site study used a commercial MRI scan simulator or
an inexpensive mock scanner for imparting behavioral training to
222 type 1 diabetic patients and age-matched healthy controls (4-10
yrs). The success rates of behavioral desensitization for obtaining a
non-sedated high-quality MRI scan reported were very high (93%
for inexpensive mock scanner and 95% for the commercial mock
scanner) [8]. Variable success rates have been reported ranging from
30 to 94% depending on the age of the children and the procedure
used [7,16-17]. Indeed, familiarizing children regarding the MRI
procedure in child-friendly settings and educational training before
the actual scan reduces distress and apprehension in children and
their families and makes the actual scanning easier [6,8].
Two secondary outcome measures also demonstrated the
usefulness of the play intervention. Blind ratings by the radiologist
indicated that the ease of diagnostic procedure was significantly
facilitated and the chances of MRI procedure being rated ‘very
easy’ increased more than 4 times in children who underwent
the play intervention activity. In addition, the caregiver level of
satisfaction with the MRI procedure was significantly enhanced for
the intervention group. Previous research has reported a decline in
anxiety among children and parents after a preparation trial with
children [18]. For example, Rothman et al. found that parental anxiety
significantly dropped after a pre-MRI intervention which comprised
of multiple interactive preparation resources (instructional booklet,
movie, and simulator practice) used with children aged 5-16 yrs [18].
Children have many unmet informational needs when they
attend hospitals and undergo clinical and diagnostic procedures.
Addressing these needs can further enhance cooperation and allay
anxiety [19]. It is important to recognize that practice with mock
MRI scanners combined with play-based activity, like the one we
have used; although useful are costly in terms of time and manpower
resources. Keeping some of these constraints in mind, newer research
has now shifted to designing internet-based tools with some measure
of success [920-21]. For example, Ashmore et al. have developed
the virtual reality app which via videos presents the child with a
panoramic view of the entire MRI procedure [9]. Such technologies,
which are freely accessible, provide immense opportunities to further
improve the quality and outreach of the pediatric neuroimaging
services. Culturally relevant educational materials or internet based
preparatory videos can be another option for wider applicability of
use across ages. Clearly, there is a need to develop innovative, cost effective,
non-invasive, and accessible strategies to reduce sedation
and distress in children undergoing pediatric radiology procedures.
The study has several strengths including a strong design, rigorous implementation of random allocation, and concealment
thereby significantly reducing the confounding and selection bias.
Even though blinding the intervention from the treating team and
the investigator was not feasible, the radiologist team was blinded to
the group allocation. Secondly, the sample size was adequate with a
nearly balanced distribution of children in the two groups. Finally,
children included in the study represented a relatively homogenous
age group with an easily documentable and objective outcome of
sedation. Indeed, there are several indirect benefits of having such an
ongoing educational and training program for children undergoing
radiological diagnostic investigations as it increases awareness about
the risks associated with use of general anesthesia on a regular basis
to the pediatric and radiological staff who are associated with this
program [16,22]. The main limitation of the study is the baseline
imbalance in the distribution of children from different socioeconomic
strata in the two groups. Possibly, this may have underestimated the
benefits of the intervention as most children from the intervention
arm were from the higher socioeconomic groups.
In conclusion, the study underscores the need for using a childcentric
approach in diagnostic testing as this considerably improves
family satisfaction and quality of neuro-imaging in the pediatric
population. Future extensions of this work should investigate the
positive impact of having an ongoing educational program regarding
the risks associated with general anesthesia in pediatric centres, and the
feasibility of using play-based strategies for imaging across different
clinical populations including children with neurodevelopmental
disorders.
Key Messages:
What is Already Known?
1. The distress that children experience during the MRI procedure
can lead to restlessness and excessive crying contributing to
poor quality imaging and delays in diagnosis and treatment.
2. U sing child-friendly techniques to reduce distress before medical
procedures and surgery is routinely used in the West; however,
their use in India is limited.What this Study Adds?
1. Child-centric play techniques improve quality of neuro-imaging
in young children undergoing diagnostic radiological investigations.
2. U sing child-friendly techniques to reduce distress among young
children before medical procedures is possible even in busy
pediatric centres.
Contributions of the Authors: BB, PM, and AKS conceived and
designed the study. BB and PM trained PPK to conduct the study.
BB and PM analyzed and interpreted the data. PM drafted the
manuscript. All the authors critically reviewed the manuscript and
are responsible for the final approval of the manuscript.