Case Report
Neuroborreliosis Manifesting with Multiple Cranial Neuropathies
Joseph S1,2 and Taimur Malik M1,2*
1Department of Neuroscience, Geisinger Neuroscience Institute, United States
2Deparment of Neurology, Geisinger Commonwealth School of Medicine, United States
*Corresponding author: Taimur Malik M, Assistant Professor of Neurology, Geisinger Neuroscience Institute 100
N. Academy Ave.Danville, PA 17822,Tel: 570-271-6590; Fax: 570-271-5874; Email: mmalik@geisinger.edu
Article Information: Submission: 29/12/2020;
Accepted: 23/03/2021;
Published: 26/03/2021
Copyright: © Joseph S, et al. This is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
It is imperative to rule out neuroborreliosis in a patient presenting with multiple cranial neuropathiesinaLyme endemic area to prevent long term
complications associated with the disease. Interpretation of serological tests is critical. With a recent history of tick bite and positive IgM antibodies, some
patients do not have the IgG antibodies against Lyme within 30 days of the exposure. Doxycycline effectively treatsLyme disease but must be given for 28
days.
Keywords
Neuroborreliosis; Multiple cranial neuropathies; Doxycycline
Introduction
Neuroborreliosis is a common manifestation of Lyme disease,
usually presents with facial nerve weakness, but other cranial nerves
can also be affected. It is essential to rule out other causes of multiple
cranial neuropathies before starting the treatment to prevent further
complications. About 5-10% of the patient would present with cranial
neuropathies [1].
Case Report
A 48-year-old female with no significant past medical history
presented to an outside hospital with a one-weekhistory of
progressive bilateral facial weakness, increased lacrimation, and
difficulty chewing. As per the patient, she was in her usual state of
health when she noticed a tick bite about two weeks back. She initially
started having a dull bilateral occipital headache after the tick bite,
which later resolved after a few days. She denies having any recent
fevers,weight loss, sensory or motor weakness in her extremities,
or altered awareness. At presentation, her vital signs were stable.
General physical examination was unremarkableexcept for difficulty in sensorineural hearing in both ears.Neurological examination
revealed dis-conjugate gaze,bilateral lower motor neuron facial
nerve weakness, and sensorineural hearing loss. Her basic labortary
investigations including complete blood, comprehensive metabolic
profile, chest x ray, urine analysisdid not show any abnormality,
while the Lyme testing showed a positive IgG/IgM antibody value
of 7.28 with 1 IgG and 3/3 IgM positive antibodies. The significant
IgM bands were 23,39,41. She later underwent an MRI (magnetic
resonance imaging) of the brain with and without contrast,which
showed enhancement of bilateral facial nerves( canalicular segments),
bilateral trigeminal nerves (cisternal segments), and left cochlear
nerve ,as shown in Figure 1B,1E,1F. A spinal tap showed normal CSF
(cerebral spinal fluid) protein and glucose with 1 white cell, while the
bacterial, viral, and fungal cultures were negative for any infectious
etiology. Patient was diagnosed with neuroborreliosis secondary to
her positive tick bite history, serological testing, and imaging findings.
She was later started on Doxycycline 100 mg twice a day for 28 days,
withclose follow-up scheduled in the neurology outpatient setting.
The patient did not have the follow-up MRI imaging yet.
Discussion
Lyme disease is a tick-borneillness caused by Borrelia burgdorferi.
About 15% of the patients infected with Lyme disease will have
neurological manifestations, including 7th cranial nerve palsy, painful
radiculopathy, and meningitis [2]. Careful history about the tick
exposure and appearance of erythema migrans (bulls-eye rash) are
important clues for the correct diagnosis. The accurate interpretation
of the serological testsis important to ensure that proper treatment is
instituted to prevent long-term complications to prevent mortality
and morbidity.
Although there is a broad differential diagnosis for multiple cranial
neuropathies which include vascular causes likebrain stem infarcts,
cavernous sinus thrombosis, intracranial aneurysms, vasculitis,
traumatic causes including skull-based fractures, intracranial
dissection, autoimmune conditions like multiple sclerosis, sarcoidosis,
acute inflammatory demyelinating polyneuropathy including
Guillain-Barré syndrome (GBS) and Miller Fisher variant,infectious
etiologies including Human ImmunodeficienyViurs (HIV), varicellazoster,
neurosyphilis, chronic fungal meningitis, neoplastic causes
like brain stem glioma’s, leptomeningeal carcinomatosis,metastatic
tumors, metabolic causes like thyroid ophthalmopathy, thiamine
deficiency and Melkersson-Rosenthal syndrome [3]. In our patient,
we excluded these differentials with the help of an MRI of the brainas
shown in Figure 1. CBC, urine analysis and CSF analysis were negative
for any infectious etiology but positive for lyme serology with a spinal
tap showinga protein of 45 and normal glucose, normal metabolic
profile with normal liver and kidney function tests.
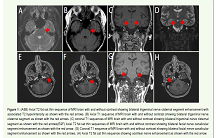
Figure 1: (A&B) Axial T2 fat sat thin sequence of MRI brain with and without contrast showing bilateral trigeminal nerve cisternal segment enhancement with
associated T2 hyperintensity as shown with the red arrows. (B) Axial T1 sequence of MRI brain with and without contrast showing bilateral trigeminal nerve
cisternal segment as shown with the red arrows. (C) coronal T1 sequences of MRI brain with and without contrast showing bilateral trigeminal nerve cisternal
segment as shown with the red arrows(E&F) Axial T2 fat sat thin sequences of MRI brain with and without contrast showing bilateral facial nerve canalicular
segment enhancement as shown with the red arrow. (G) Coronal T1 sequence of MRI brain with and without contrast showing bilateral facial nerve canalicular
segment enhancement as shown with the red arrows. (H) Axial T2 fat sat thin sequence showing cochlear nerve enhancement as shown with the red arrow.
As per the previousguidelines from the Center of DiseaseControl
(CDC), a two tier testing is recommended which include to have an
initial enzyme-linked immunosorbent assay(ELISA) testing for the specific antigens, and if the sample is positive or borderline positive
it undergoes Western blot testing to confirm the diagnosis. If 5/10
specific IgG bands are present in patients with symptoms of more
than 30 days or 2/3 IgM bands present with symptoms of less than 30
days, the Western blot is considered positive [4].
A new modified two-tier testing algorithm has also been
approved by the CDC, which is as accurate as the standard two-tier
testing utilizing only the enzyme immunoassay (EIA). If the initial
test is positive, another EIA is performed to confirm with a different
set of antigens [5,6]. Prompt treatment with Doxycycline 200 mg
daily for 2-4 weeks or in a patient who is allergic to Doxycycline,
Amoxicillin 1.5 gm daily is considered effective, while Azithromycin
or Clarithromycin can be used if an alternative agent is needed.
Ceftriaxone 2 gm daily is also viewed efficacious [7,8].
It is important to have a broad differential in a patient with
multiple cranial neuropathies patient, but a concise history, optimal
serological markers and imaging need to be done to prevent longterm
complications.