Case Series
Diffusion Restriction: Its Diverse Implications in the Pediatric Brain
Panchal V, Rajat Arora R* and Rathod Y
Department of Radiodiagnosis and Imaging, Government medical college and new civil hospital, Surat, Gujarat, India
*Corresponding author: Rajat Arora, Senior resident, Department of Radiodiagnosis and Imaging, Government medical college and new civil hospital, Bunglow no. 2, behind kapadia health club, janta nagar-B, New civil road, Surat, India; E-mail: rajatarora180@gmail.com
Copyright: © 2020 Panchal V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Information: Submission: 27/09/2020; Accepted: 27/11/2020; Published: 30/11/2020
Abstract
We present a case-series of 6 cases, which shows the different implications of the finding of diffusion restriction and how this finding, in combination with the clinical history and other relevant MR findings points out to a diagnosis in completely different spectra, which therefore has significant impact on the patient management.
Keywords
Diffusion restriction; Pediatric
Introduction
We present a case series of 6 cases, showing diverse etiopathogenic spectrum in the underlying pathologic mechanism of the diffusion restriction seen on DWI images with corresponding hypointensity seen on ADC maps.
The spectrum includes infarctions (arterial as well as venous), auto
regulatory disorders like PRES, global hypoxia and hypo perfusion
(HIE), trauma (DAI), Infections (TB, pyogenic abscess), Toxic and
metabolic disease (Mitochondrial disorders, hypoglycemia, urea
cycle defects), Demyelination (ADEM, MS) and neoplasm (Gliomas,
medulloblastomas, Choroid plexus tumors etc.).
Diffusion-Weighted Imaging (DWI) has also become a pillar of
current neuroimaging. Diffusion abnormalities represent alterations
in the random movement of water molecules in tissues, revealing
their micro architecture, and occur in many neurological conditions.
DWI provides useful information, increasing the sensitivity of MRI
as a diagnostic tool, narrowing the differential diagnosis, providing
prognostic information, aiding in treatment planning and evaluating
response to treatment.
DWI provides image contrast that is dependent on the molecular
motion of water.
Diffusion abnormalities represent alterations in the random
movement of water molecules in tissues, revealing their micro
architecture, and occur in many neurological conditions [1]. In a
DWI sequence diffusion sensitization gradients are applied on either
side of the 180° refocusing pulse. The parameter “b value” decides
the diffusion weighting and is expressed in s/mm2. It is proportional
to the square of the amplitude and duration of the gradient applied.
Diffusion is qualitatively evaluated on trace images and quantitatively
by the parameter called Apparent Diffusion Coefficient (ADC).
Tissues with restricted diffusion are bright on the trace image and
hypo intense on the ADC map. In the brain, factors contributing
to the measured ADC include true random diffusion, tortuosity of
the diffusion space, cytosolic streaming, exchange times between
compartments and restriction by cell membranes
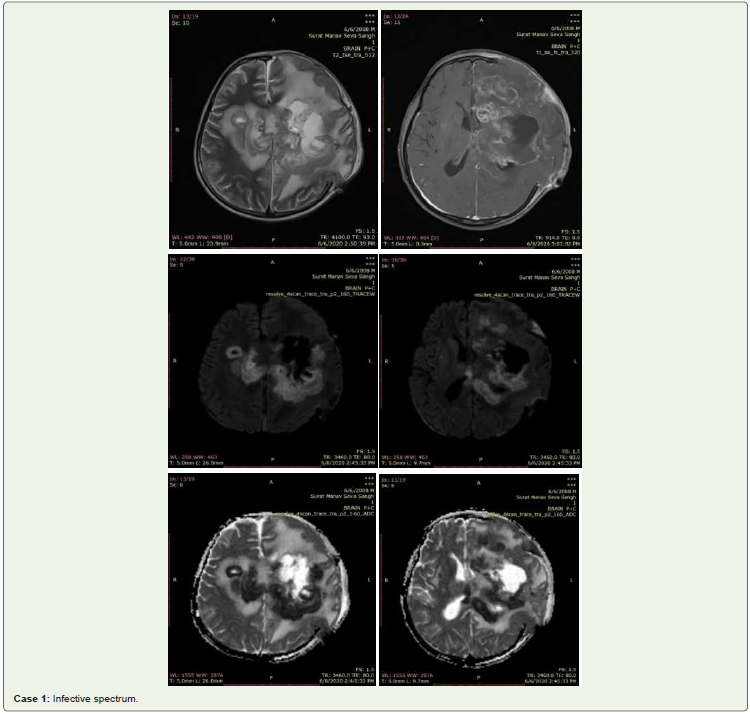
Case 1
This patient was an 8 years old child who presented with c/o
fever and seizures and was advised MRI-Brain study; MRI revealed multiple conglomerate T2-hypointense lesions which show diffusion
restriction in left front parietal region, basal ganglia, body of corpus
callosum, right centrum semiovale, with perilesional vasogenic edema
seen. Most of these showed peripheral post contrast enhancement.
These were diagnosed as Infective Tuberculomas and Tubercular
abscesses, which was confirmed on histopathology. The patient
responded well to ATT
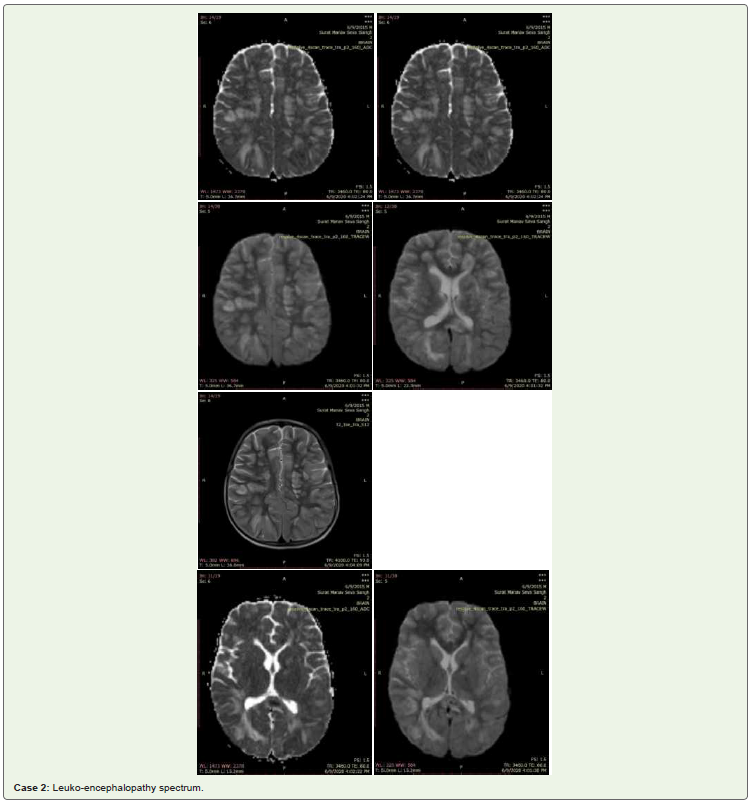
Case 2
These images show multiple T2-FLAIR hyper intense lesions
in bilateral centrum semiovale, corona radiata, corpus callosum
as well as in the subcortical and periventricular white matter with
diffusion restriction seen in splenium of corpus callosum in a 5 years
old child with c/o fever, altered sensorium. Findings were s/o acute
leukoencephalopathy
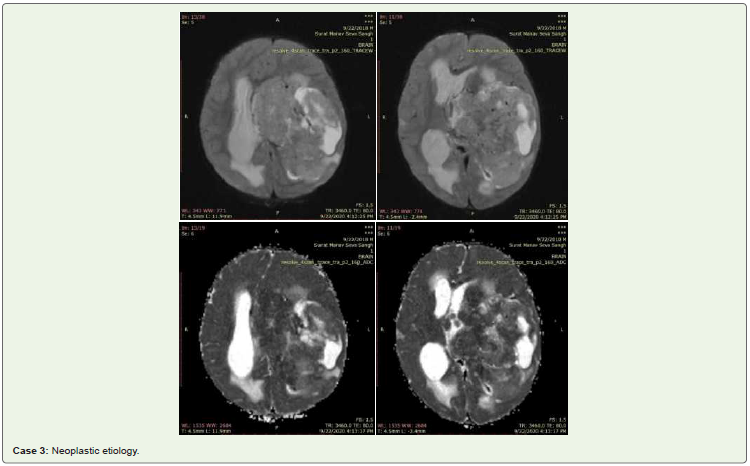
Case 3
These sets of DWI-ADC images of an infant with altered
sensorium show a large lobulated solid-cystic lesion in the temporal,
occipital horns and body of lateral ventricle on left side, with the solid
component showing patchy diffusion restriction. It causes mass-effect
with midline shift of 12 mm towards right side and is infiltrating into
the left temporoparietal neuroparenchyma. The lesion was diagnosed
as a malignant neoplastic etiology of choroid plexus origin, Choroid plexus carcinoma. The radiological diagnosis was corroborated with
histopathological diagnosis obtained post-surgical excision.
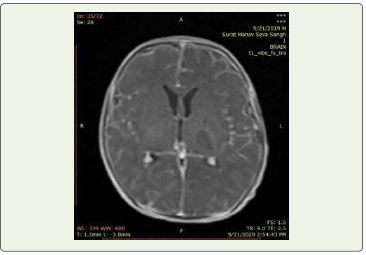
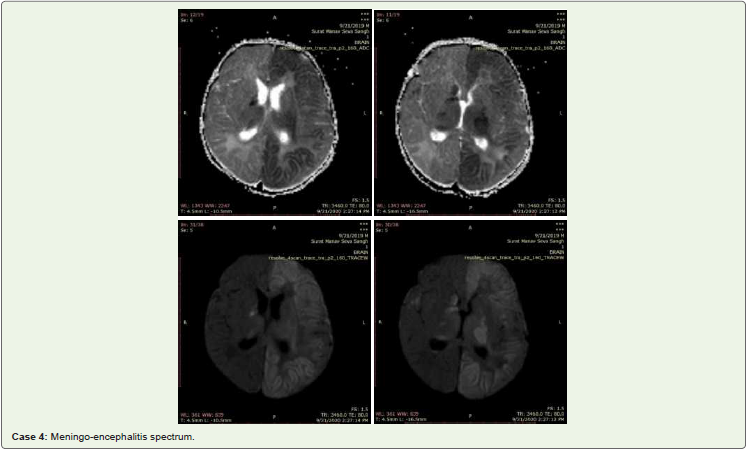
Case 4
The patient was a 6 years old pediatric patient, who presented
with fever, nuchal rigidity and vomiting; CSF analysis revealed
leucocytosis with differential neutrophilia and low CSF sugar levels;
These images show diffusion restriction in left cerebral hemisphere,
left basal ganglia, bilateral thalami mainly involving the cortex (i.e.
gray matter) with partly involving subcortical white matter; Such a
pattern of restriction differentiates infarct from encephalitis; Infarct
involves loss of GM-WM differentiation with diffusion restriction, as
opposed to the cortical restricting pattern seen here.
The child responded well to intravenous antibiotics.
Additionally, T1 Post contrast images show exaggerated
meningeal enhancement without abnormal enhancement of the
cortex or basal ganglia, Represents changes of meningo-encephalitis.
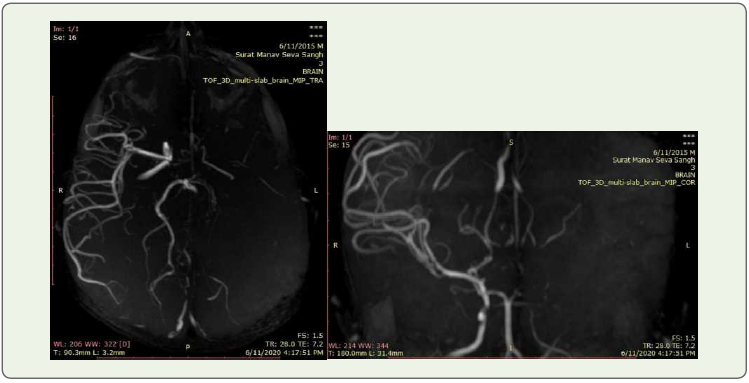
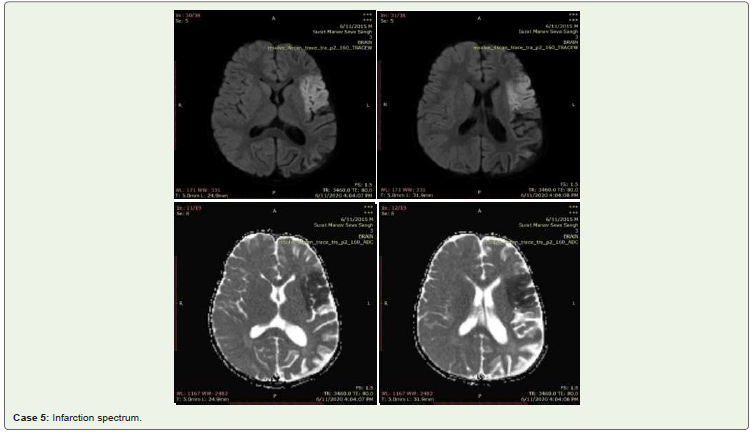
Case 5
This patient was 4 year old child who presented with right sided
hemiplegia; MRI study revealed an ill-defined area of diffusion
restriction with corresponding low ADC value in left frontal region
and insular cortex (Perisylvian distribution). No e/o any blooming
foci seen on GRE.
Represents acute non-haemmorhagic infarct.
Additionally gyral thinning with sulcal space widening seen in left
cerebral hemisphere, s/o left sided hemi-atrophy
Left sided MCA, PCA and right ACA were not visualized, s/o
complete thrombosis.
Possible differentials were Hemiconvulsion Hemiplegia Epilepsy
Syndrome (HHE) more likely Moya –moya like disease, less likely.
Follow-up work up for ruling out Moya-Moya revealed no
supportive finding; The child later also went on to develop seizures
also, which confirmed the diagnosis of HHE.
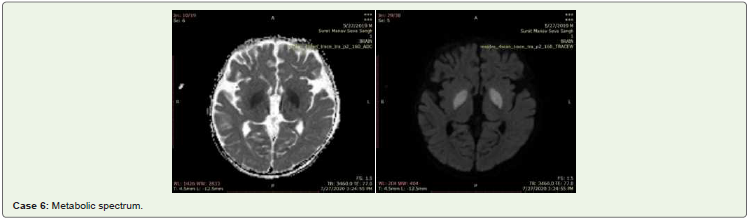
These images shows diffusion restriction in bilateral Globus
pallidus, in an infant who presented with seizures and excessive
drowsiness. Initially diagnosed with?encephalitis clinically,
Biochemical investigations revealed Hyperammonemia with
deranged LFTs. Final diagnosis of metabolic encephalopathy (Acute
hyperammonemic encephalopathy).
Case 6
The child responded well to the supportive treatment for hyperammmonemia.
Discussion
The clinical presentation in different pediatric neurological
conditions is extremely various, depending on age, cause, and
involved vascular territory, any metabolic abnormality associated
Therefore the radiologiocal findings have to be clinically correlated
for an accurate diagnosis.
The practical applications of DWI are in identifying regions and
patterns of abnormal DWI signal and further characterizing them to
low or high ADC’s values.
The same finding of diffusion restriction in a patient with
hemiparesis implies infarction. Conversely the same finding in a
patient with seizures, fever could represent encephalitis spectrum,
which includes both infective as well as auto-immune mediated. In a
patient with systemic metabolic disorders (E.g hepatic dysfunction),
the same finding would imply metabolic encephalopathy.
Hematological/vascular disorders (like sickle, moya-moya) may
present with stroke like picture with TOF-Angiography sequences
showing the underlying etiopathology.
Among the pediatric strokes, embolic stroke tends to present
suddenly, whereas thrombosis may have a more gradual onset.
Focal neurologic deficits (cranial nerve palsies, hemiparesis, and
hemisensory loss) are the most common presentation of AIS in
children. Seizures, headache, language and speech difficulties, and
altered mental status are also possible.
Based on these cases, it can be inferred that all the cases show
more/less similar neuro-radiological picture on DWI-ADC imaging
and therefore interpretation of all their differentials should be done
in the clinical setting of presentation; All these cases are differential
diagnosis to each other as far as the radiological picture is concerned;
Diffusion-Weighted Imaging (DWI) is a well-established
technique in neuroimaging, but the diagnostic value of DWI
outside the setting of acute infarct and abscess is sometimes underrecognised
particularly in paediatric neuroimaging. DWI also plays
an important role in the evaluation of intracranial infection, brain
tumours, demyelinating diseases, and metabolic disorders.
DWI was more sensitive than the other MR sequences in detecting
early pathological changes even in cases of viral encephalitis and
leukodystrophy apart from ischemia. It was also helpful in delineating
the area more accurately at the microscopic level.
Conclusion
Pediatric neuroradiological finding of diffusion restriction should therefore, be interpretated according to the clinical scenario of presentation, and in unison with the additional findings seen on other sequences such as GRE, T1-T2-FLAIR and post contrast sequences, to arrive at the final diagnosis.
The step-wise imaging algorithm for pediatric should be the diagnostic imaging paradigm with which radiologists and clinicians alike approach these patients. MRI is the initial modality of choice, including shortened stroke protocols (e.g. DWI, ADC, and SWI/GRE), followed by vascular imaging to detect abnormalities which may underlie an identified stroke.