Review Article
Capsular Enhancement in Hepato Cellular Carcinoma - A Short Review
Rajasree P, Patnaik S*, Uppin S and Varma SRC
Nizam’s Institute of Medical Sciences, Hyderabad, India
*Corresponding author: Patnaik S, Nizam’s Institute of Medical Sciences, Hyderabad, India
Copyright: © 2020 Rajasree P, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Information: Submission: 11/03/2020; Accepted: 14/04/2020; Published: 16/04/2020
Introduction
Carcinoma (HCC) is the most common primary
malignancy and the most common cause of cancer-related death
among patients with chronic liver disease. Hepatitis B and C infections
are recognised risk factors. Other risk factors are hepatic fibrosis due
to metabolic diseases like hemochromatosis, Wilson’s disease, biliary
cirrhosis and aflatoxins etc. Every year approximately 350,000 new
cases are diagnosed in the world [1,2]. It is more common in 60-70
yrs of age group with a male predominance. Serum alfa fetoprotein
is a helpful laboratory test for initial screening. Several imaging
modalities like USG, CT SCAN, MRI, PET CT have largely replaced
biopsy for diagnosis. Dynamic multiphase CT and contrast MRI are
the imaging modalities of choice. Functional imaging like perfusion,
diffusion weighted images, elastography give additional information
for characterisation, diagnosis, treatment and follow up. A recent
AASLD statement recommended that tumors more than 1cms with
typical enhancement pattern on dynamic CT need no biopsy [3].
Early diagnosis of HCC by imaging is desirable, as various treatment
options like liver transplantation, segmental resection and local
ablation therapy can be offered early leading to better outcome [4].
Imaging features:
The HCC can be macroscopically classified into 3 main patterns.
The most common is expansile single nodular, well defined,
encapsulated with better prognosis, seen in 50% cases. Another
variety is infiltrative lesions without capsule and frequently has
vascular invasion. The third one is multifocal lesions in multiple liver
segments [5]. Microscopically it ranges from well differentiated to
undifferentiated. Radiologically it may present as massive focal mass/
multinodular or diffuse.Diverse CT findings of HCC like mosaic pattern, venous invasion,
tumor capsule, intra-tumoral abnormal vessels and arterioportal
shunting have been reported [6]. However typical HCC shows
arterial phase enhancement and wash out in portal venous and or
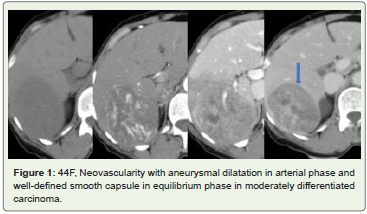
in equilibrium phase in contrast enhanced CT and MRI (Figure 1). Capsular enhancement in portal or in equilibrium phase is an
important diagnostic feature of HCC. A fibrous capsule frequently
observed around the tumor during growth. Even according to LIRADS,
the major features of HCC are arterial phase enhancement,
size of lesion, portal venous phase wash out, enhancing capsule in
portal-venous phase/delayed /equilibrium phase and spread of tumor
over a threshold [7].
The Capsule:
A capsule is defined as a smooth continuous area along
the periphery of the lesion that had different attenuation than
surrounding liver as opposed to ring enhancement. On MDCT the
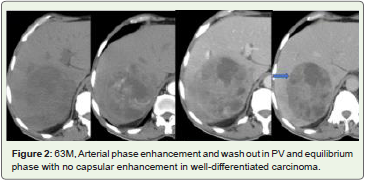
capsule appears as curvilinear border surrounding at least half of the tumor. Capsule appearance is noted in 43 to 64% cases (Figure 2 and 3)
[8,9]. This capsular appearance is seen in portal venous /equilibrium
phase and appears as thick capsule. Arterial phase enhancement
and capsular enhancement are major diagnostic criteria of HCC.
Histologically fibrous capsule has inner layer of fibrous tissue and
outer layer of portal venules and newly formed bile ducts. There are
many hypotheses for fibrous capsule formation- one is because of
passive thickening of liver stroma due to compression pressure of
liver parenchyma; other it may be due to defence reaction of liver
stroma to restrain mechanical injury caused by the tumor nodule
[10]. This capsule represents a zone where the tumor communicates
with adjacent parenchyma.
Figure 1: 44F, Neovascularity with aneurysmal dilatation in arterial phase and
well-defined smooth capsule in equilibrium phase in moderately differentiated
carcinoma.
The capsule is formed by host of mesenchymal cells and not
by HCC. Since the capsule formation is result from interactions
between the tumor and host liver, it interferes with the growth and
invasion of HCC [11]. This is supported by clinical evidence that
prognosis of patient with HCC having capsule is better than those
without capsule [12]. Majority of HCC in cirrhotic liver are well
circumscribed and encapsulated whereas in non- cirrhotic liver are
infiltrative. Fibrolamellar HCC show heterogenous enhancement in
late arterial phase with evidence of non-enhancing central scar. It
becomes isodense to rest of adjacent parenchyma in portal venous
phase and wash out in equilibrium phase as seen in classic HCC in
noncirrhotic liver. Capsular enhancement when present, it is seen in
equilibrium phase and they have discontinuous capsule in 35% cases
[13]. Development of HCC in cirrhotic liver is a multiphase processstarting
from regenerative nodule to low grade dysplastic nodule to
high grade dysplastic nodule with subsequent progression to HCC focus in dysplastic nodule giving rise to ‘nodule within nodule’
pattern. These changes occur in early phase HCC which subsequently
progress to high grade HCC. When a nodule is dysplastic the normal
arterial flow is reduced, and venous flow is maintained. With
development of HCC there is arterialisation of blood supply and
sinusoidal capillarization develops. There are new unpaired arteries
which are not accompanied by bile ducts. Gradually the number of
unpaired arteries increase which is proportionately increase with
differentiation of HCC, particularly size less than 3 cms.
Figure 2: 63M, Arterial phase enhancement and wash out in PV and equilibrium
phase with no capsular enhancement in well-differentiated carcinoma.
Figure 3: 63M, Intense homogenous arterial phase enhancement; Wash out
in PV with corona enhancement in late arterial phase; Thin smooth capsular
enhancement in equilibrium phase in well-differentiated carcinoma.
Typical CT features are not always observed in all HCC. In
their study Lee et al observed that 56.4% of cases showed typical
enhancement. It is also observed that 62.6% of moderately
differentiated, 35.4% of well-differentiated, 52.3% of poorly
differentiated HCC show classical pattern [14]. Well differentiated
tumors receive portal blood flow whereas moderately differentiated
tumors, poorly differentiated tumors, as well as tumor larger than
3cms are supplied by arterial blood [15].
Significance of capsular enhancement:
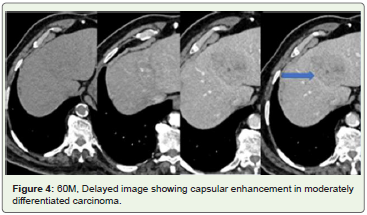
Formation of fibrous capsule, which is a smooth, uniform and
enhancing rim surrounding most of the nodules is a prominent
feature of HCC (Figure 4). Presence of capsule indicates progressive
HCC, not degenerative or regenerative nodules [16]. It is absent
in early HCC and develop as a barrier for spread of tumor cells.
Gradually it disappears due to tumor cell invasion. Hence its
presence indicates tumor progression [17]. Since the significance of
this capsular enhancement is not well-high-lighted in literature. We
have analysed the capsular pattern in 5 cases of histopathologically
proven Hepatocellular carcinoma (3 well differentiated, 2 moderately
differentiated tumor) and discussed its importance in its evaluation.
Capsular enhancement is seen 4 of 5 cases.Differential diagnosis:
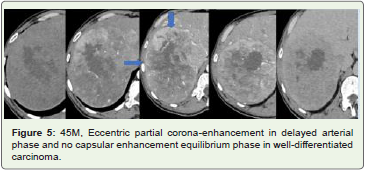
Pseudo-capsule: Capsule is to be differentiated from pseudocapsule which is peri-tumoral fibrosis and sinusoidal dilatation. This pseudo-capsule is thinner and show less enhancement. The distinction
between capsule and pseudocapsule can only made in pathology. In at risk patients the capsular appearance has high predictive value of HCC regardless whether the rim enhancement represent capsule or pseudocapsule. 90% of HCC more than 5 cms in Asian population and 40% of non- Asians show capsule [18]. Presence of capsule or pseudocapsule differentiate HCC from dysplastic/regenerative nodules. Fibrous capsule in HCC indicates favourable prognosis as it is associated with more effective trans-arterial chemo embolization and lower recurrence after resection or ablation due to barrier effect of tumor dissemination [17,19].Corona enhancement: Capsular enhancement has also to be differentiated from corona enhancement which is due to transient rim enhancement of hypervascular HCC in arterial phase (Figure 5). This is due to vascular drainage of HCC. As the tumor cells proliferate rapidly the intra nodular and peri-nodular venous
blood drains into surrounding sinusoid. Fibrous capsule that acts as a barrier gets interrupted and intra-tumoral blood drain into surrounding parenchyma via portal venules of the capsule. Hence, corona enhancement is seen in late arterial or portal phase when most of tumor show reduction of enhancement, not seen in equilibrium
phase when the fibrous capsule enhances. It of variable in thickness and may be circumferential or eccentric or non-symmetric. This sign if present indicates HCC. This area corresponds to drainage pathway of tumor cells. Hence, this is the site of tumor recurrence or intrahepatic metastasis or daughter nodule [20].
Conclusions
Capsular enhancement is an interesting imaging finding, that can
be observed in a significant number of HCC. Its true significance is
not well-described in literature. Its clinical implication and the need
to differentiate from pseudo-capsule are high-lighted in this review.