Case Report
Black Bronchoscopy: A Case of Uncommon Active Mycobacterial Tuberculosis Presentation
Lakshmi K1, Vijaya P2, Raghava SP3* and Soma S4
1Department of Pulmonology, Lalitha Super Specialities Hospital, India
2Department of Neurology, Lalitha Super Specialities Hospital, India
3Department of Cardiology, Lalitha Super Specialities Hospital, India
4Department of Internal Medicine, Lalitha Super Specialities Hospital, India
*Corresponding author: Raghava SP, Lalitha Super Specialities Hospital, Guntur, Andhra Pradesh-522001, India, Mobile no: +91 9440800355; E-mail: drpvraghav@gmail.com
Copyright: © 2020 Lakshmi K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Information: Submission: 13/01/2020; Accepted: 20/03/2020; Published: 23/03/2020
Abstract
Bronchial anthracofibrosis was first encountered during the nineteenth century. In that era, this clinical entity was found to be a consequence of
occupational exposure. Although still an infrequent finding, diverse etiologies of this finding have emerged. We describe an unusual finding of black mucosal
pigmentation in a 15-year-old boy triggered by active tubercular infection.
Keywords
Bronchial anthracofibrosis; Bronchoscopy; Mycobacterial tuberculosis
Introduction
Anthracofibrosis refers to bronchoscopic narrowing accompanied
by black mucosal pigmentation. The term was first coined by Chung et
al. in 1998 whilst delineating the clinical features of this phenomenon
in 28 patients [1]. Earlier observations associated anthracofibrosis
with occupational exposure due settlement of soot and coal particles
on bronchial mucosal and submucosal layers. Furthermore, cases
observed in elderly Asian women were justified by prolonged wood
smoke exposure due to the tradition of cooking on wood fires [2].
However, less familiar causes of anthracofibrosis have recently been
documented in current literature. Here, we describe a case of ‘black
bronchoscopy’ in a 15-year-old boy prompted by active tubercular
infection.
Case Report
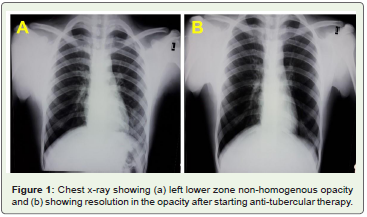
A 15-year-old young boy presented for an evaluation of cough of one day duration and a hemoptysis bout of approximately 200 ml. The patient denied any occupational or biomass fuel exposure. He also did not have any past history of tuberculosis or tuberculosis medication. Chest x-ray revealed non-homogenous opacity
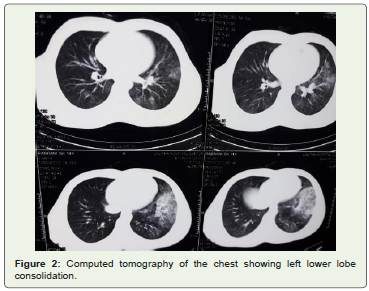
occupying the left lower zone (Figure 1a). Computed Tomography (CT) of the chest revealed area of consolidation occupying the antero-medial segment of left lower lobe (Figure 2). In view of these findings, work-up was started for detection of infectious causes particularly tuberculosis and also to determine the immune status of the patient, with arrangements for bronchoscopy. The Acid- Fast
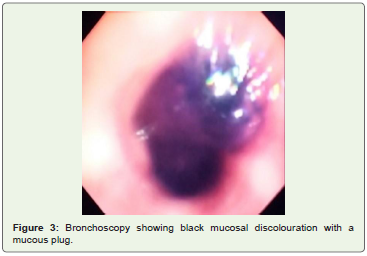
Bacilli (AFB) and Human Immunodeficiency Virus (HIV) tests were both negative. Bronchoscopy displayed an area of mucosal black pigmentation with a black coloured mucous plug obstructing the left lower lobe bronchus (Figure 3). The mucous plug was cleared and bronchial washings and brushings from the same area were collected. The collected specimens were sent for Cartridge-Based Nucleic Acid Amplification Test (CBNAAT), AFB staining, fungal culture, and cytology. The CBNAAT report detected rifampicin sensitive Mycobacterium Tuberculosis (MTB), AFB staining was positive, fungal cultures were negative, and cytology was negative for malignant cells as well as anthracotic pigments. The patient was then advised BACTEC-MGIT, which grew MTB, thus confirming the diagnosis of active tuberculosis. The patient was started on antitubercular
therapy consisting of isoniazid, rifampicin, pyrazinamide and ethambutol. Repeat chest x-ray of the patient showed resolution in the size of the area of consolidation in the left lower zone, indicating response to therapy (Figure 1b). Informed consent was obtained from the guardian of the patient.
Figure 1: Chest x-ray showing (a) left lower zone non-homogenous opacity
and (b) showing resolution in the opacity after starting anti-tubercular therapy.
Discussions
Previous literature evidences bluish-black discolouration of the
bronchial mucosal lining accompanied by stenosis, as a sequel of
ruptured necrotic foci from enlarged lymph nodes in both active and
healed tuberculosis. This clinical entity has been termed as bronchial
Anthracofibrosis [1]. Knowledge accumulated over the years have
revealed the association between bronchial anthracofibrosis and
tuberculosis [3]. Despite absence of both stenosis and enlarged lymph
nodes in our patient, black mucosal pigmentation was still observed.
We suspected a diagnosis of tuberculosis in our patient and therefore
performed CBNAAT, AFB, fungal culture, and cytology tests.
Although, AFB, fungal and cytology tests were negative a diagnosis
of tuberculosis was confirmed due to the growth of MTB cultures.
A similar case was reported by Kala et al. in which both AFB and
Mantoux yielded negative results despite growth of MTB cultures [4].
Bronchial anthracofibrosis has been predominantly observed
in elderly female patients. This finding is attributable to history of
prolonged wood smoke exposure specific to this population subset.
Additionally, bronchial anthracofibrosis displays a propensity to
affect the right middle lobe, followed by the right upper, left upper,
right lower, and left lower lobe of the bronchial tree [1,3,5]. Contrary
to these frequent observations, Inaty et al. described consolidation
of the superior left lower lobe in a male patient [6]. Similarly, we
also detected consolidation of the left lower lobe in a 15-year-old
male patient. However, tuberculosis as an associated condition of
anthracofibrosis, rather than a causative agent has been reported
in literature [7,8]. This association could explain anthracofibrosis
findings in males with affected bronchial regions other than the right
middle lobe.
Active tuberculosis may be challenging to diagnose due to atypical
clinical presentation in some patients [1]. Chung et al. and Fortis et al.
reported the absence of typical symptoms such as fever and weight loss
in their patients [1,8]. Kunal et al. reported negative AFB stains and
negative Mantoux tests in 4/4 and 3/4 patients with active tuberculosis
[7], respectively. The sputum smear for AFB was also negative for our
patient. These findings indicate that a diagnosis of active tuberculosis
may frequently be missed. A definitive diagnosis may be made through
visual examination of the endobronchial tree using bronchoscopy.
Despite the need of this invasive procedure to confirm the diagnosis,
active tuberculosis should always be ruled out [7].
Although many causes of airway hyperpigmentation are benign
in nature, diagnosis of a particular cause remains crucial for optimal
treatment. In this era of increased frequency of bronchoscopic
examinations, we as pulmonologists should be aware of the differential
diagnosis of MTB infection presenting as lower lobe consolidation.
In our case, bronchoscopic examination revealed black pigmentation
of the endobronchial mucosa. Our patient responded well to antituberculous
treatment.
Conclusion
Airway hyperpigmentation even in the absence of enlarged
lymph nodes or airway stenosis should always raise the suspicion of
active mycobacterium tuberculosis as one of the differential diagnosis
for black bronchoscopy, especially in patients without occupational exposures, malignancies, house-hold fire exposure or endobronchial
ignition therapies as India is one of the leading countries burdened by
tuberculosis. Anti-tubercular treatment helps in resolving symptoms,
but airway hyperpigmentation is usually irreversible.