Case Report
Olfactory Groove Meningioma
Hussein ML1*, Mira RR2 and Mathew V1
1Hamad General Hospital, Hamad Medical Corporation, Qatar
2Geriatrics/Internal Medicine Fellow at Loyola University, USA
Corresponding author: Hussein ML, Hamad General Hospital, Hamad Medical Corporation, Doha, Qatar, Tel no: 0097433466229; E-mail: MHussein9@hamad.qa
Citation: Hussein ML, Mira RR, Mathew V. Olfactory Groove Meningioma. Indian J Appl Radiol. 2019;5(1): 131.
Copyright ©2019 Hussein ML, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Applied Radiology | Volume: 5, Issue: 1
Submission: 26/11/2018; Accepted: 03/01/2019; Published: 05/01/2019
Abstract
The most frequent primary brain tumours in adults are gliomas and primary CNS lymphomas. Meningioma represents about 30 percent of them. This tumor is usually slow-growing tumor that arises from the meninges, the membranous layers surrounding the brain and spinal cord. Symptoms depend on the location and occur as a result of the mass effect on adjacent tissue. One of these locations is subfrontal olfactory groove. These kinds of meningiomas arise from the meningeal coverings of the cribriform plate or the frontosphenoidal suture. Olfactory Groove Meningiomas (OGMs) are typically non-cancerous and account about 10 percent of all meningiomas, according to the American Brain Tumor Association (ABTA). Olfactory groove meningiomas develop insidiously and their diagnosis is commonly made late, when tumors are large. Their treatment is therefore mostly surgical. In this report, we specifically focus on the clinical presentation as well as the radiologic characteristics of this disease based on a case that has been admitted at Zawia Teaching Hospital, Libya. Furthermore we would discuss some newly recommended surgical approaches. We present this unusual case that has been diagnosed successfully by MRI.
Keywords: Brain tumor; Meningioma; Olfactory groove; Subfrontal extra axial mass
Introduction
Meningiomas account for about a third of all primary brain tumors [1]. Usually benign, typically affect men and women between the ages of 40 and 70; they are extremely rare to occur in children. They affect women more often than men [2,3]. Patient who has olfactory groove meningioma probably will not experience any symptoms until the tumor extends and grows to a large size that may cause symptoms such as loss of smell and taste, blurred vision, memory loss, headaches, fatigue, nausea and vomiting, and personality changes. On other hand, in this location if the tumor is small in size, we often do not find olfactory groove meningiomas until we perform a Magnetic Resonance Imaging (MRI) scan for an unrelated reason. OGMs are usually occurring in the midline, but as their size increases they might become asymmetric. The frontal lobes are often displaced superiorly and posteriorly, and in very larger tumors, inferior and lateral displacement of the optic nerves and chiasma are observed in some reported cases [4]. Their growth can also extend inferiorly through the cribriform plate into the ethmoid sinus, through the planum sphenoidale into the sphenoid sinus, or even laterally through the orbit. Olfactory groove meningiomas is highly vascularized tumors [5]. Their main blood supply is derived from the anterior and posterior ethmoidal arteries of the external carotid artery as well as contribution of the middle meningeal artery and meningeal branches of the ophthalmic artery.
Furthermore, hyperostosis of the nearby underlying bone is not uncommon, and might extend into ethmoid sinuses and nasal cavity can occur in 15%-25% of cases [6,7]. CT scan is recommended to exclude the hyperostosis. This is an important point because in presence of this finding it will definitely affect the plan of the management. These involved surrounding bones have to be surgically removed to improve the outcomes and decrease the rate of recurrence as we will discuss later.
The first consideration of the differential diagnoses of OGMs is the intracranial schwannomas especially that originate from the anterior ethmoidal nerve. Both CT-scan and MRI studies revealed a similar preoperative characteristic of large subfrontal tumor [8-10]. Despite close similarities with olfactory groove meningiomas, patient history and radiological findings as well as histopathological study provide substantial evidence for differential diagnosis.
Case Report
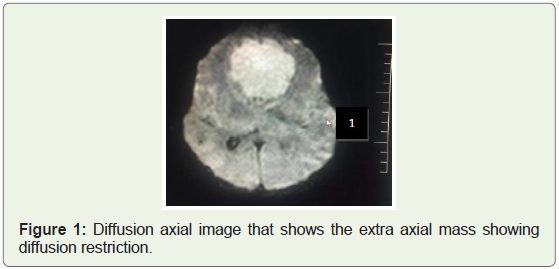
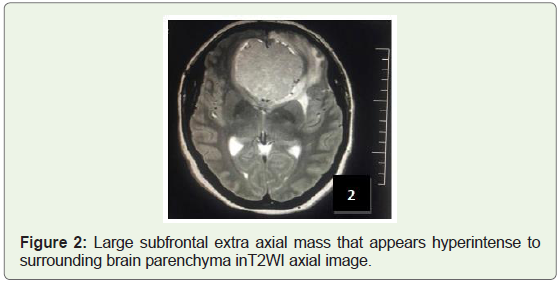
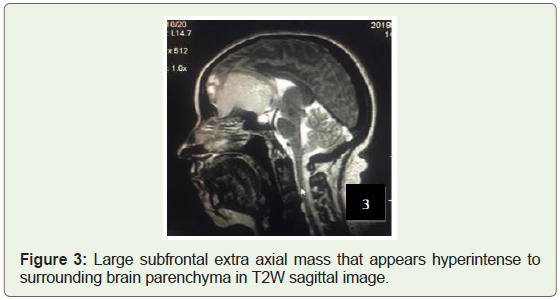
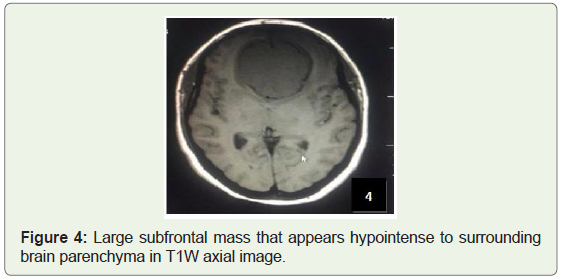
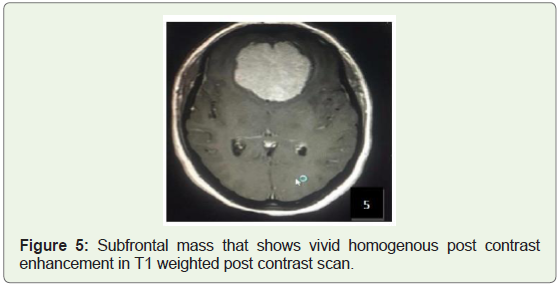
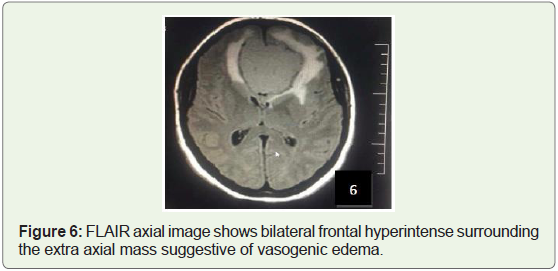
A 40-year-old female patient visited our institution who presented with a history of progressive headache, nausea and blurred vision. Magnetic Resonance Imaging (MRI) of brain revealed a large subfrontal anterior cranial fossa mass arising from olfactory groove and surrounding falx, this mass appears isointense to gray matter on T1-weighted sequences and heterogeneous iso-to hyperintense on T2-weighted sequences with diffusion restriction and vivid enhancement after administration of Gadolinium (Figure 1-5). The mass causing sever mass effect with lateral displacement of medial aspects of both frontal lobes, splayed compressed frontal horns of both lateral ventricles, and posterior displacement of genu of the corpus callosum. Moderate surrounding T2W and FLAIR signal hyperintensity within frontal lobes bilaterally representing vasogenic edema (Figure 6). MR spectroscopy was not done in this study.
According to the World Health Organization (WHO) classification, the histopathology corresponded to grade 1 meningioma. The degree of tumor removal was grade II according to the Simpson’s grading system using the bilateral subfrontal approach. Post surgical functional outcome gave the patient a score of 90 using the Kornofsky Performance Scale (KPS) and the patient was discharged on day 3. Follow-up of the patient post-surgery could not be maintained as patient did not show up for her appointments.
Discussion
WHO grades meningiomas on a scale from I to III where I is benign, II being atypical and III representing anaplastic/ malignant. Majority of the meningiomas are WHO grade I. Atypical and anaplastic meningiomas can be distinguished from type I (benign) by histopathology. Olfactory groove meningiomas account for 8 to 13% of all intracranial meningiomas. OGMs are commonly diagnosed when their size is significant and causes local pressure effect. The initial symptoms of many patients are nonspecific and slow in progression. Many individuals have asymptomatic meningiomas that have been discovered only during an autopsy. 1% to 2% of all autopsies reveal meningiomas that were unknown to the individuals during their lifetime [2,3,11]. In the 1970s, tumors causing symptoms were discovered in 2 out of 100,000 people, while tumors discovered incidentally occurred in 5.7 out of 100,000. With the advent of modern sophisticated imaging systems such as CT scans and MRI, the discovery of asymptomatic meningiomas has tripled [11]. Anosmia is one of the earliest presenting complaints, At the time of diagnosis, anosmia is noted in more than 50% of cases [4]. Later on the patients start complaining of headaches and personality changes, such as apathy and akinesia, which are commonly misleading as being associated with depression or aging. Rarely, Seizures as well as aggressiveness which has been reported as a result of frontal lobe dysfunction in some studies. Later stages of this disease can lead to dementia, urinary incontinence, nasal obstruction and epistaxis, spontaneous Cerebrospinal Fluid (CSF) leaks due to its local invasion in the paranasal sinuses add to that the visual problems resulting from compression of the optic nerve or optic chiasm or intraorbital invasion of the tumor. Less frequently patient with OGM presented as case of Foster Kennedy syndrome in which the triad of anosmia and unilateral optic atrophy with contralateral papilledema are observed simultaneously [5,12,13].
The causes of this mass is not well known. Some scientific studies indicating that the Genetic alterations play an important role. The most frequent genetic mutations about 50% involved in meningiomas are inactivation mutations in the neurofibromatosis 2 gene (merlin) on chromosome 22q. Other mutations such as TRAF7 are present in about 25% of meningiomas. Mutations in the TRAF7, KLF4, AKT1, and SMO genes are commonly expressed in benign skullbase meningiomas. Mutations in NF2 are commonly expressed in meningiomas located in the cerebral and cerebellar hemispheres [14].
The differential diagnosis of a large and enhancing subfrontal mass in adult are olfactory groove meningiomas and subfrontal schwannomas. Schwannomas of the ethmoidal nerve are very rare and it is hard to be distinguished from meningiomas by imaging only [4]. One of the reported studies mentioned that the distinction point between schwannoma and meningioma is the nearby bone state. Schwannomas cause a little more bony erosion, whereas meningiomas tend to cause hyperostosis. Furthermore subfrontal schwannomas were exceeding rarely reported so we did not expect this tumor to be a schwannoma [5]. Neuroblastoma, squamous cell carcinoma, adenocarcinoma, and metastases should also be considered in the differential diagnosis in adults with a tumor involving both the nasal cavity [12,13].
Imaging is useful in making the diagnosis and to evaluate suspected intracranial tumors. Although MRI is the imaging test of choice as it reveals the soft tissue tumors, meningiomas should be seen using Computed Tomography (CT scan) using contrast as well. The CT scan shows any associated bony hyperostosis while bony involvement is important to determine, as it highly contribute to tumor recurrence [8,15]. Olfactory groove meningiomas tend to have a rather high rate of recurrence (30% at 5 years and 41% at 10 years), which is mainly because incomplete resection, particularly of the involved underlying bone at the cranial base [16-18].
Many different surgical interventions have been recommended based on evidence of cure. Resection has traditionally been performed using a bifrontal or pterional approach, both of which require some degree of brain retraction or manipulation to expose the tumor that affecting the general outcomes [18-20]. On the other hand, the purely endoscopic endonasal transcribriform approach that has been done and reported in certain studies. This approach as they had mentioned offers a direct midline trajectory and immediate access for removal of olfactory groove meningiomas without brain retraction and manipulation of neurovascular structures. Extracapsular dissection with preservation of the arachnoid planes can be achieved using bimanual microsurgical techniques through a keyhole craniectomy directed at the ventral skull base. In carefully selected patients, complete Simpson Grade I tumor removal including the dural attachment and involved hyperostotic bone can be achieved. Excellent panoramic visualization of the entire ventral skull base extending from the posterior wall of the frontal sinus to the planum sphenoidale can be obtained with a 30° endoscope after performing a modified Lothrop procedure. Successful cranial base reconstruction can be performed using a multilayer fascia lata and AlloDerm technique supplemented by bilateral vascularized nasoseptal flaps. During the surgical operation, the adjacent paranasal sinuses increases the risk of CSF leakage and meningitis [18,20-22]. Thus, most surgeons have taken a more conservative approach, usually prefer to use a Simpson Grade II resection, without aggressive resection of the involved bone at the cranial base to avoid these complications. However, cauterization of the dural or resection alone without removal of bone involvement leads to high rate of recurrence [6,7,22].
References
- National Cancer Institute (2016) Adult Central Nervous System Tumors Treatment.
- Ferri F (2017) Ferri’s Clinical Advisor 2018: 5 Books in 1(1st edn.). Elsevier Health Sciences pp: 809.
- Wiemels J, Wrensch M, Claus EB (2010) Epidemiology and etiology of meningioma. J Neurooncol 99: 307-314.
- Kim SH, Lee JH, Sung SK, Choi CH (2017) Subfrontal schwannoma extended broadly to nasal cavity treated by gamma knife radiosurgery following surgical excision: A case report. Brain Tumor Res Treat 5: 116-119.
- Kim DY, Yoon PH, Kie JH, Yang KH (2015) The olfactory groove schwannoma attached to the cribriform plate: a case report. Brain Tumor Res Treat 3: 56-59.
- Liu JK, Christiano LD, Patel SK, Tubbs RS, Eloy JA (2011) Surgical nuances for removal of olfactory groove meningiomas using the endoscopic endonasal transcribriform approach. Neurosurg Focus 30: E3.
- Bakay L (1984) Olfactory meningiomas. The missed diagnosis. JAMA 251: 53-55.
- Sauvaget F, François P, Ben Ismail M, Thomas C, Velut S (2013) Anterior fossa schwannoma mimicking an olfactory groove meningioma: case report and literature review. Neurochirurgie 59: 75-80.
- Lotfipour S, Chiles K, Kahn JA, Bey T, Rudkin S (2011) An unusual presentation of subfrontal meningioma: A case report and literature review for Foster Kennedy syndrome. Intern Emerg Med 6: 267-269.
- Zachariah SB, Khoromi S (2009) Meningioma, sphenoid wing: differential diagnoses and workup. eMedicine.
- Lee JH (2008) Meningiomas: Diagnosis, Treatment, and Outcome. Springer Science & Business Media pp: 3-13.
- Kanaan HA, Gardner PA, Yeaney G, Prevedello DM, Monaco EA, et al. (2008) Expanded endoscopic endonasal resection of an olfactory schwannoma. J Neurosurg Pediatr 2: 261-265.
- Bezircioğlu H, Sucu HK, Rezanko T, Minoğlu M (2008) Nasal-subfrontal giant schwannoma. Turk Neurosurg 18: 412-414.
- (2012) Meningioma. Mayo Clinic.
- Hentschel SJ, DeMonte F (2003) Olfactory groove meningiomas. Neurosurg Focus 14: 1-5.
- Bakay L, Cares HL (1972) Olfactory meningiomas. Report on a series of twenty-five cases. Acta Neurochir (Wien) 26: 1-12.
- Mathiesen T, Lindquist C, Kihlström L, Karlsson B (1996) Recurrence of cranial base meningiomas. Neurosurgery 39: 2-7.
- Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL (1985) Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg 62: 18-24.
- Nakamura M, Struck M, Roser F, Vorkapic P, Samii M (2007) Olfactory groove meningiomas: clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery 60: 844-852.
- Obeid F, Al-Mefty O (2003) Recurrence of olfactory groove meningiomas. Neurosurgery 53: 534-543.
- Persky MS, Som ML (1978) Olfactory groove meningioma with paranasal sinus and nasal cavity extension: a combined approach. Otolaryngology 86(5): ORL-714-ORL-720.
- Pieper DR, Al-Mefty O, Hanada Y, Buechner D (1999) Hyperostosis associated with meningioma of the cranial base: secondary changes or tumor invasion. Neurosurgery 44: 742-747.