Case Report
Cervical Ectopic Pregnancy with Cervical Placental Invasion. A Case Report of a Rare Entity: Diagnosis and Management
Elmahdy A1, Yousef R2, Badr SS2, Al-Obadli A2, Szmigielski W3*, Elkady B4, Ashwini G2, Ibrahim AA5 and Manal T5
1Radiology Resident, Hamad General Hospital, Hamad Medical Corporation, Qatar
2Department of Clinical Imaging, Women’s Hospital, Hamad Medical Corporation, Qatar
3Department of Clinical Imaging, National Center for Cancer Care and Research, Hamad Medical Corporation, Qatar
4Radiology Resident, Badr Healthcare Directorate, Egypt
5Department of Obstetrics and Gynecology, Women’s Hospital, Hamad Medical Corporation, Qatar
Corresponding author: Szmigielski W, Department of Clinical Imaging, National Center for Cancer Care and Research, Hamad Medical Corporation, P.O. Box - 3050, Doha, Qatar, Tel no: 00974-66556368; E-mail: w.szmigielski@gmail.com; wszmigielski@hamad.qa
Citation: Elmahdy A, Yousef R, Badr SS, Al-Obadli A, Szmigielski W, et al. Cervical Ectopic Pregnancy with Cervical Placental Invasion. A Case Report of a Rare Entity: Diagnosis and Management. Indian J Appl Radiol. 2018;4(1): 123.
Copyright ©2018 Elmahdy A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Applied Radiology | Volume: 4, Issue: 1
Submission: 11/05/2018; Accepted: 04/07/2018; Published: 09/07/2018
Abstract
Cervical ectopic pregnancy is a rare variant of ectopic pregnancy. It has an incidence of less than 1% of all ectopic pregnancies. It is associated with a high morbidity and mortality potential.
Method: We are reporting one case of ectopic cervical pregnancy at 11+ weeks. Because this condition carries high risk, early diagnosis and management is extremely important. The role of Ultrasound and Magnetic Resonance Imaging in the diagnosis has been discussed.
Conclusion: US and Magnetic Resonance Imaging play important role in the diagnosis of Cervical Ectopic pregnancy.
Keywords: Pregnancy complications; Cervical pregnancy; Magnetic Resonance Imaging (MRI); Ultrasonography
Background
Cervical pregnancy is an ectopic pregnancy in which the gestational sac implants in the cervical canal. The incidence of cervical pregnancy is rare (< 1% of ectopic pregnancies) [1].
Cervical pregnancy carries a high risk of life-threatening bleeding if it is not treated correctly. Risk factors include previous endometrial curettage, previous cesarean section, use of intrauterine devices, and assisted reproductive technologies. If the diagnosis is delayed, massive bleeding or even hypovolemic shock may occur [2].
Cervical pregnancy is rarely diagnosed before 20 weeks’ of gestation. Accurate early diagnosis and critical decision-making are of great importance in the management of this condition, since they allow treatment with minimal intervention and attenuate the overall rates of morbidity and mortality [3].
Early diagnosis and medical management with systemic or local administration of methotrexate is the treatment of choice. If the pregnancy is disturbed, it may lead to massive hemorrhage, which may require hysterectomy to save the patient [4].
We report a case of Cervical Ectopic Pregnancy diagnosed by Transabdominal Ultrasound and Magnetic Resonance Imaging of the Pelvis at 11+ weeks of gestation.
Case
In this study, we present the case of a 33-year-old primigravida patient, with no past medical illnesses or past surgical procedures. Other relevant history included amenorrhea of 11 weeks duration with a positive urine pregnancy test. She presented on 25 February 2018 at 11+ weeks complaining of on and off uncomfortable sensation in the lower abdomen and brownish vaginal spotting. The patient’s vital signs were stable and on examination the abdomen was soft, lax and non-tender. Hemoglobin level at presentation was 12.8 g/dL.
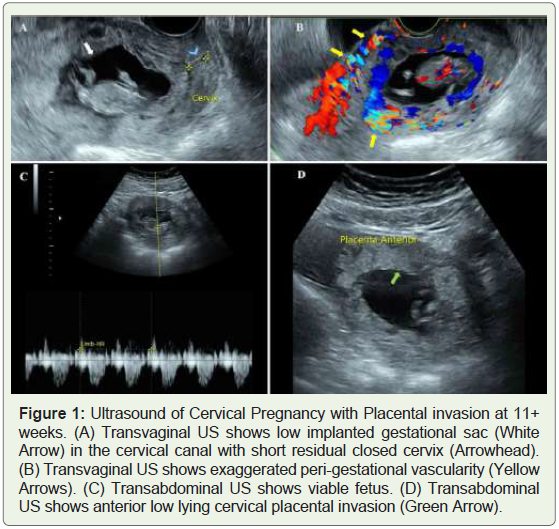
Ultrasound, both transabdominal and transvaginal, was performed on 25 February 2018 and it revealed a low implanted gestational sac seen in the cervical canal with short residual closed cervix length, measuring 9 mm (Figure 1A). According to the Crown-Rump Length (CRL) of 4.9 cm, the calculated gestational age was 11 weeks and 5 days. Peri-gestational high vascularity was noted (Figure 1B). Fetal heart beats and fetal movements were seen and recorded (Figure 1C). A low lying placenta was noted encroaching on the anterior cervical wall which was suggestive of anterior placental invasion (Figure 1D). A presumptive diagnosis of Cervical Placenta was made.
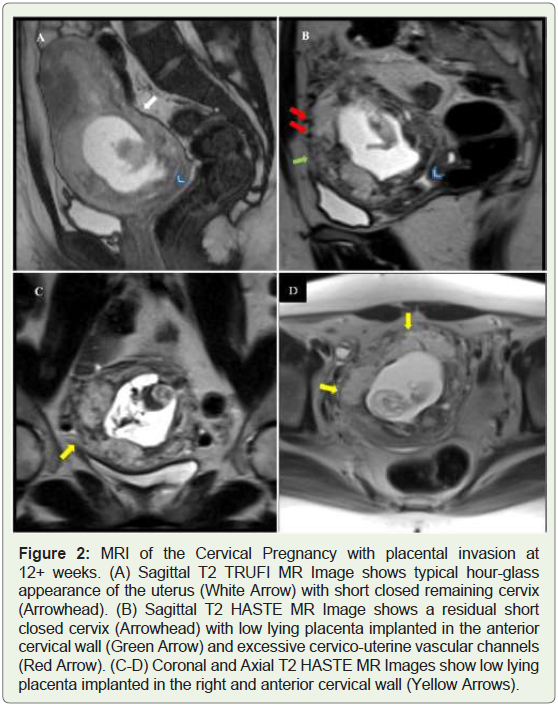
Non-Contrast Magnetic Resonance Imaging (MRI) of the pelvis using multiphase sequences in different planes was performed on 04 March 2018. It revealed a gravid uterus showing the typical hourglass configuration with gestational sac and fetus seen inside, located at cervico-uterine region (Figure 2A). Residual short closed cervix was seen, measuring 8 mm with low lying placenta seen implanted in the anterior right cervical wall with excessive cervico-uterine vascular channels (Figure 2B,2C).
The diagnosis of Ectopic Cervical Pregnancy was made with suggested placenta increta. A Multi-Disciplinary Team (MDT) meeting was held, which consisted of the OBGYN team, vascular surgeon, urologist, anesthetist and radiologist. The plan was made advocating conservative treatment rather than surgical management.
On 05 March 2018, intra-amniotic feticide was pursued with ultrasound-guided intra-amniotic instillation of potassium chloride (KCL). B-hCG at this time was 39,926 mIU/mL.
On 11 March 2018, following confirmation of normal liver and renal function, an intramuscular methotrexate injection was administered.
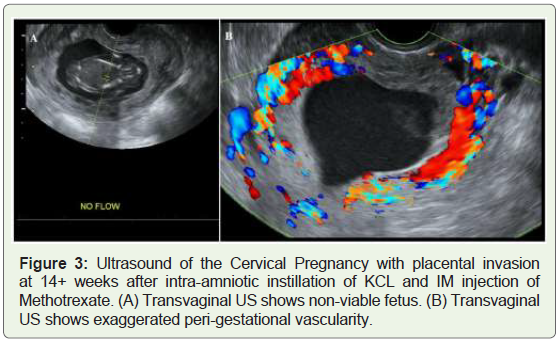
Transvaginal ultrasound performed on 14 March 2018 showed a non-viable fetus with no recorded heartbeats (Figure 3A). It showed the low implanted gestational sac in the cervical canal with high perigestational exaggerated vascularity (Figure 3B). B-hCG at this point was 7,443 mIU/mL.
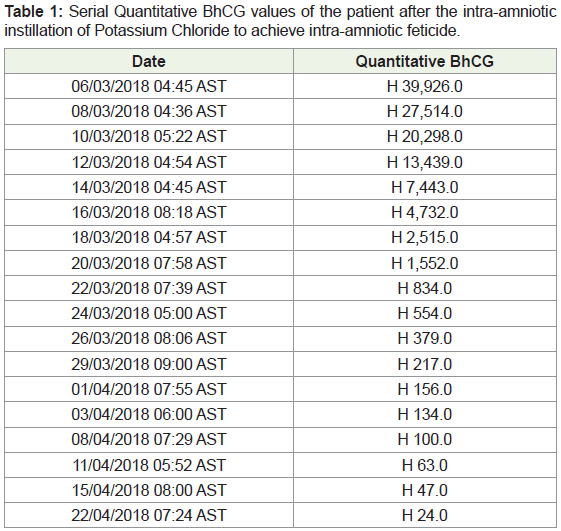
A close follow up of the patient was done for more than one month with serial B-hCGs to check for level drop and serial ultrasound examinations to check the peri-gestational vascularity (Table 1).
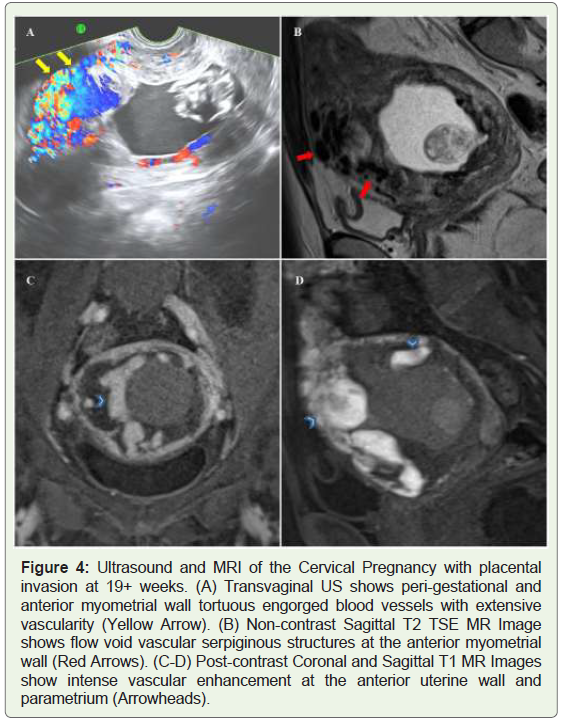
Transvaginal US performed on 22 April 2018 showed extensively increased vascularity with tortuous engorged vessels at the anterior myometrial wall, which was suggestive of a developing Arteriovenous Malformation (AVM) (Figure 4A).
Multiplanar, multisequence Magnetic Resonance Imaging (MRI) of the pelvis with and without Gadolinium contrast medium was performed on 24 April 2018. It showed the anterior placenta implanted into right and anterior cervical wall, with multiple vascularlike serpiginous structures at anterior uterine wall, endometrial cavity and parametrium characterized by flow void on T1 and T2 (Figure 4B). On contrast enhanced dynamic sequences, the multiple vascularlike structures showed intense enhancement (Figure 4C,4D). Findings were confirmative of arteriovenous fistula.
On 02 May 2018, the patient underwent fluoroscopic-guided bilateral Internal Iliac Artery angioembolization. On the same day, the patient was shifted to the OR for suction evacuation of the products of conception. This was accompanied by insertion of Bakri balloon catheter and cervical cerclage. Estimated blood loss during the operation was 3.5 L so, the patient was transfused 5 units of PRBCs and 2 units of FFP. The patient was vitally stable and Hemoglobin level postoperatively was 10 g/dL.
Discussion
Cervical pregnancy is a rare type of ectopic pregnancy, which results from implantation of the gestational sac within the cervical canal [5]. Transvaginal ultrasound or MRI is used for early diagnosis of cervical pregnancy [6].
According to Ushakov, et al. who reviewed 117 cases of cervical pregnancy, sonography improved pretreatment diagnosis up to 81.8% [7]. The following findings of transvaginal ultrasound indicate a cervical pregnancy: a gestational sac or placental tissue visualized within the cervix or a cardiac motion noted below the level of the internal os with a closed internal os. There will be no intrauterine pregnancy and the uterine shape becomes “hourglass” with an enlarged cervix. If there is peri-trophoblastic blood flow under color Doppler ultrasound, a cervical ectopic pregnancy must be considered.
Vela, et al. reported 12 cases of patients with cervical pregnancy and none of the 12 patients with the correct initial diagnosis required a hysterectomy [8]. Therefore, the earlier the correct diagnosis is made, the less complications are likely. This emphasizes the importance of the early diagnosis of a cervical pregnancy.
Different treatment methods have been described for termination of CP (Cervical pregnancy). Often more than one method is tried in the termination [9]. Treatment methods for CP can be divided into five categories [10]:
1. Tamponade with Foley catheter: Use of a Foley catheter, placed gently past the external os, followed by inflation of the bulb with 30 mL saline has been used mostly after other techniques (e.g., curettage), result in hemorrhage. Tamponade with packing is not very useful.
2. Reduction of blood supply: This may be undertaken by cervical cerclage, vaginal ligation of cervical arteries, uterine artery ligation, internal iliac artery ligation and angiographic embolization of the cervical, uterine or internal iliac arteries. This is usually done in preparation for surgical therapy like curettage, or along with chemotherapy, as a conservative treatment modality aimed at preserving future fertility. Embolization is primarily used as a “rescue” therapy when profuse bleeding follows other conservative methods like chemotherapy.
3. Surgical excision of trophoblast: Curettage and hysterectomy are the classic methods for surgical excision of trophoblast tissue. Curettage is the age-old fertility preserving method, but risks hemorrhage. Therefore, it has been used in conjunction with mechanical methods like cervical artery ligation and tamponade. Primary hysterectomy may still be the preferred modality of treatment in intractable hemorrhage, second trimester or third trimester diagnosis of CP and possibly to avoid emergency surgery and blood transfusion in a woman not desirous of fertility. In a review, 100% of CP beyond 12 weeks’ gestation ultimately required hysterectomy.
4. Intra-amniotic feticide: Ultrasound-guided intra-amniotic instillation of potassium chloride and/or methotrexate has been used as a conservative approach for the management of CP. Both these procedures require skill and expertise.
5. Systemic chemotherapy: The most commonly used agent is methotrexate, used in a single dose or multiple doses, with or without folinic acid [10]. Treatment with methotrexate chemotherapy of patients with either viable or nonviable CP at < 12 weeks’ gestation carries a high success rate (> 91%) for preservation of the uterus [11].
In our case, the primigravida patients presented before 12 weeks with brownish vaginal spotting and lower abdominal discomfort. Transabdominal and Transvaginal Ultrasonography were suggestive of cervical pregnancy. MRI of the pelvis confirmed the diagnosis. The patient was offered conservative measures rather than surgical management. Intraamniotic feticides with systemic Methotrexate chemotherapy were offered. US follow up revealed no significant decrease in the peri-gestational vascularity and eventually AV Malformation. This raised the possibility of intractable bleeding that may lead to hysterectomy if curettage was attempted at that stage. Thus, Uterine Artery Embolization (UAE) was successfully performed after which the patient underwent surgical curettage for excision of the trophoblastic tissue. This was accompanied by Balloon Tamponade and Cervical Cerclage.
Conclusion
Cervical pregnancy is a rare condition that is seldomly reported because of risk factors like high cesarean section rate and increased use of assisted reproductive technique for management of infertility. The success of conservative treatment depends on the timely and prompt diagnosis by early Ultrasound and Magnetic Resonance Imaging, which can reduce the chances of severe life-threatening hemorrhage necessitating hysterectomy or blood transfusion.
References
- Kochi K, Hidaka T, Yasoshima K, Yoneda K, Arai K, et al. (2014) Cervical pregnancy: a report of four cases. J Obstet Gynaecol Res 40: 603-606.
- Chang H, Chiu T, Hsieh T, Lo L (2014) Early cervical ectopic pregnancy: A case report and review of the literature. J Med Ultrasound 22: 117-119.
- Hasanzadeh M, Rezaee MAM, Sherafati G, Azad A, Mirtaymore M (2016) Cervical ectopic pregnancy with placenta percreta and gross hematuria: A Case Report. J Midwifery Reprod Health 4: 631-634.
- Samal SK, Rathod S (2015) Cervical ectopic pregnancy. J Nat Sci Biol Med 6: 257-260.
- Jaswal TS, Singh S, Nanda S, Sangwan K, Chauhan M, et al. (2002) Cervical ectopic pregnancy with placenta percreta and bladder wall invasion. Acta Obstet Gynecol Scand 81: 991-992.
- Adabi K, Nekuie S, Rezaeei Z, Rahimi-Sharbaf F, Banifatemi S, et al. (2013) Conservative management of cervical ectopic pregnancy: Systemic methotrexate followed by curettage. Arch Gynecol Obstet 288: 687-689.
- Ushakov FB, Elchalal U, Aceman PJ, Schenker JG (1997) Cervical pregnancy: past and future. Obstet Gynecol Surv 52: 45-59.
- Vela G, Tulandi T (2007) Cervical pregnancy: The importance of early diagnosis and treatment. J Minim Invasive Gynecol 14: 481-484.
- Leeman LM, Wendland CL (2000) Cervical ectopic pregnancy: Diagnosis with endovaginal ultrasound examination and successful treatment with methotrexate. Arch Fam Med 9: 72-77.
- Singh S (2013) Diagnosis and management of cervical ectopic pregnancy. J Hum Reprod Sci 6: 273-276.
- Kung FT, Chang SY (1999) Efficacy of methotrexate treatment in viable and nonviable cervical pregnancies. Am J Obstet Gynecol 181: 1438-1444.