Research Article
Vesico-Vaginal Reflux – A Less Recognised Entity
Chandan G, Kulkarni AM* Gouri N, Ravishankar PM and Asif M
Department of radio-diagnosis, S. S. Institute of Medical Sciences and Research Centre, India
Corresponding author: Kulkarni AM, Department of radio-diagnosis, S. S. Institute of Medical Sciences and Research Centre, Davangere, Karnataka, India, Tel no: +91-9008735596; E-mail: drakhilkulkarni@gmail.com
Citation: Chandan G, Kulkarni AM, Gouri N, Ravishankar PM, Asif M. Vesico-Vaginal Reflux – A Less Recognised Entity. Indian J Appl Radiol. 2018;4(1): 121.
Copyright © 2018 Chandan G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Applied Radiology | Volume: 4, Issue: 1
Submission: 02/01/2018; Accepted: 02/04/2018; Published: 05/04/2018
Abstract
Vesicovaginal Reflux (VVR) is a rarely encountered and less known entity among paediatricians and radiologists. It is a functional voiding disorder, usually seen in pre-pubertal girls without anatomical or neurological abnormality and is defined as abnormal retrograde reflux of urine into vaginal vault during bladder distension and early micturition. It presents with vaginal collection sonographically identical to obstructive hydrocolpos. It is important to differentiate these two, as the treatment of VVR is mainly non-surgical.
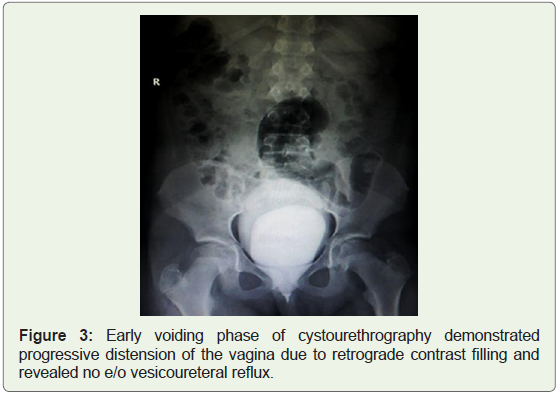
Aims and objectives: The purpose of this study was to describe a series of cases of adolescent girls presenting with various genitourinary symptoms where sonography showed a vaginal collection similar to hydrocolpos, later proved to be due to VVR. The protocol for diagnosis and findings of VVR are reviewed based on multiple imaging modalities (Table 1).
Materials and Methods: With the informed consent by patients, 200 girls aged between 8-18 years having recurrent genitourinary symptoms were examined and sonographically imaged. Of these, 5 children who had sonologically detectable vaginal collection were evaluated in full bladder status and postvoid status. Few additional investigations like IVU, MCU, CT urography and MRI were done to rule out anatomical abnormalities of the genitourinary tract.
Results: Findings common to these was a well defined ovoid vaginal collection identified in full bladder that disappeared after complete voiding. Additional imaging modalities ruled out anatomic abnormalities of the genitourinary tract.
Conclusion: Vesicovaginal reflux can produce vaginal collection that is sonographically identical to obstructive hydrocolpos. It is important to differentiate this functional disorder presenting as hydrocolpos from other obstructive causes of hydrocolpos which require surgical management. Sonographic examination in distended bladder followed by a postvoid evaluation easily provides the correct diagnosis of VVR by demonstrating disappearance of the vaginal collection. Management includes behavioural modifications, toilet training and parental education.
Keywords: Vesicovaginal reflux; Hydrocolpos; Vaginal collection; Urinary incontinence; UTI; Sonography
Introduction
Vesico-Vaginal Reflux (VVR) is a rarely encountered and less known entity among paediatricians and radiologists. It is a functional voiding disorder, usually seen in pre-pubertal girls without anatomical or neurological abnormality and is defined as abnormal retrograde reflux of urine into vaginal vault during bladder distension and micturition. It presents with vaginal collection mimicking hydrocolpos. The clinical spectrum varies from asymptomatic bacteriuria to recurrent Urinary Tract Infection (UTI), postvoid dribbling, wetting, frequency, urgency, day time enuresis and genital infections. Imaging protocol should include sonographic evaluation in full bladder and postvoid evaluation for correct diagnosis of this entity. Additional imaging modalities such as voiding cystourethrography, Intravenous urography, CT scan and MRI studies can be done to rule out any anatomical defects of the urogenital tract. It is important for the radiologist to be aware of this entity so as to differentiate this functional disorder presenting as hydrocolpos from other obstructive causes of hydrocolpos which require surgical management. We report our experience in 5 cases of vesicovaginal reflux.
Material and Methods
The Study was carried out in two institutions, Adichunchanagiri Institute of Medical Sciences, Karnataka and Prince Ali Khan Hospital, Mumbai. The study was given ethical clearance from the ethical committees of both the institutions.
200 girls aged between 8 to 18 years, who presented to the pediatric department with repeated urinary tract infection, post void dribbling, day time enuresis, frequency or urgency and genital infections were evaluated by a non-invasive protocol, including a careful history, physical examination, neuro-urologic examination, urine analysis and transabdominal sonographic evaluation. Standard imaging protocol included sonographic evaluation of abdomen and pelvis in full urinary bladder. In cases where sonography showed fluid filled collection posterior to bladder suggestive of hydrocolpos were sonographically imaged again following complete micturition. Few suitable additional imaging modalities like Intravenous urography, micturating cystourethrogram, CT urography and MRI were conducted in these patients. On confirming the diagnosis, these patients were effectively managed and followed up once in 3 months for clinical symptomatology for the next one year.
Result
In our study the patients are of the age between 8-12 years. These patients presented with the complaints of urinary tract infection and few patients also presented with additional symptoms of nocturnal enuresis and dribbling of urine. In addition, all these patients also had recurrent episodes of UTI with an average of 4-5 episodes per year.
Pre void sonography in all patients revealed retro vesicle vaginal collection and post void sonography revealed disappearance of vaginal collection. The patients were diagnosed with VVR and managed. Follow up of patients after one year revealed no further episodes of UTI.
Discussion
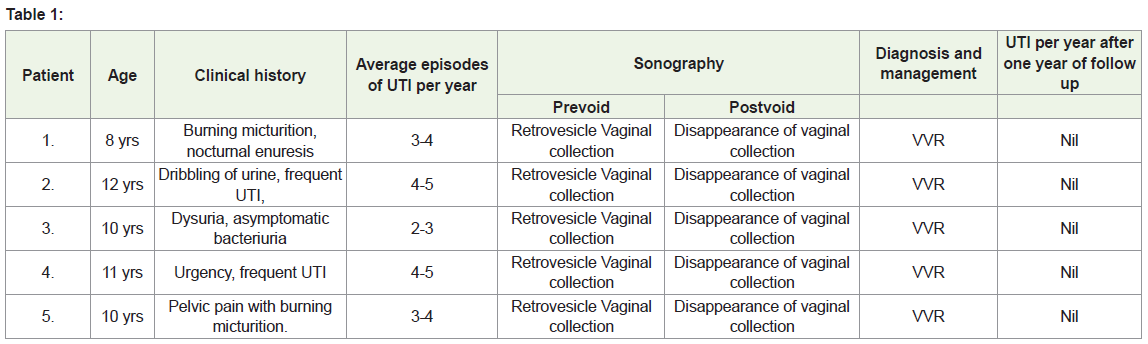
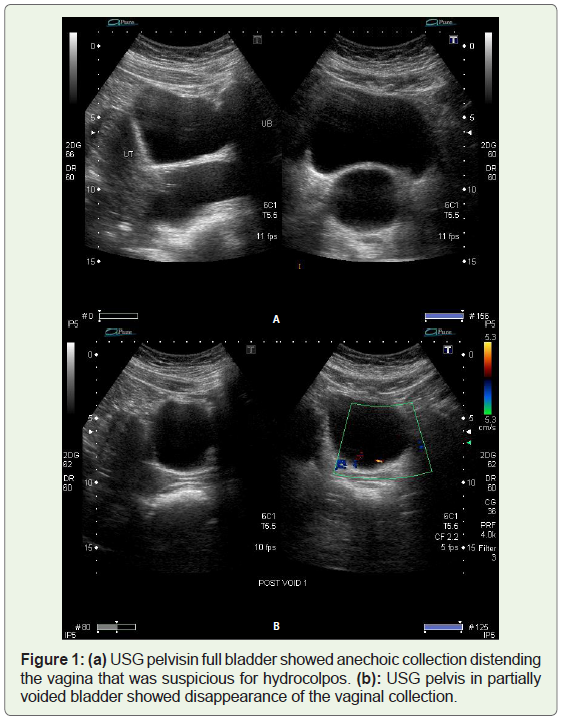
Hydrocolpos is a rare finding in pediatric population. It usually results from anatomical vaginal obstruction as in case of imperforate hymen, septate vagina, hypoplastic vagina, vaginal stenosis and other complex genitourinary malformation like ectopic ureter [1]. Non obstructive causes of hydrocolpos include leaking amniotic fluid in pregnant patients, erroneous placement of a Foley’s catheter into the vagina and abnormal accumulation of urine [2]. Vesicovaginal reflux is a rare cause of hydrocolpos in pre pubertal girls occurring without any anatomical obstruction. It can occur both in supine and upright position [3]. The exact cause for VVR is not clear. Many hypotheses to explain the mechanism of VVR have been proposed in the literature. Large labia majora, labia minora adhesions or their tight apposition may result in retrograde tracking of urine into the vagina behind the hymen [4-6]. Obesity and behavioural factors like infrequent voiding or abnormal voiding position are contributory to the development of VVR. Many functional abnormalities such as cerebral palsy, spastic pelvic floor musculature have also been attributed to cause VVR. VVR is a rare cause of recurrent urinary tract infection in pre-pubertal girls. Other common presenting symptoms include daytime incontinence, nocturnal enuresis, vulvovaginitis, bad urinary smell and nonspecific pelvic pain [1,7]. It is the abnormal collection of urine in the vagina when bladder is over distended, which mimics hydrocolpos (Figure 1a). However, unlike hydrocolpos it disappears completely following complete voiding (Figure 1b ). It has been described in literature as retrograde filling of the vagina during full bladder and micturition followed by complete emptying of the vagina after voiding [7]. The interesting point noticed in our cases was that the hydrocolpos was present when the bladder was over distended (Figure 2). Since hydrocolpos is responsible for significant amount of residual volume and subsequent development of UTI, avoiding the development of hydrocolpos could reduce the frequency of UTIs. This can be done by advising the children for frequent urination, so as to avoid over distension of bladder and the development of hydrocolpos. The same was advised in all our patients and were followed up for one year. It was found out that the number of episodes of UTIs was significantly reduced in all the patients.
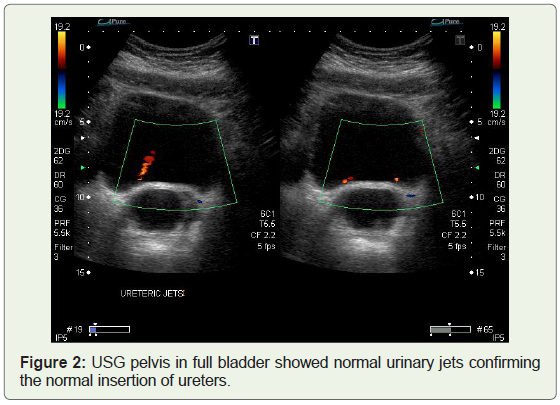
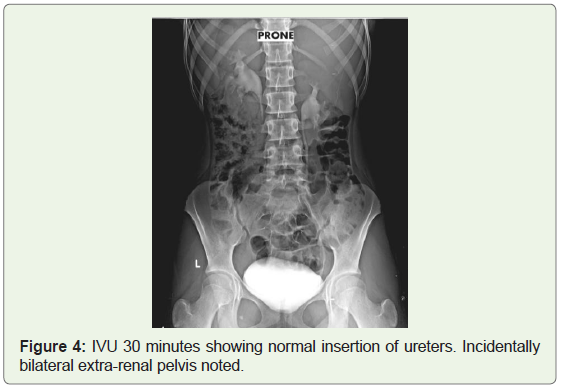
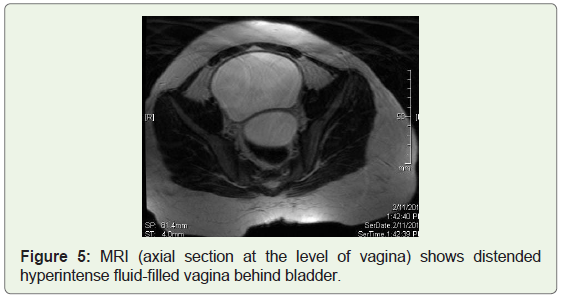
The diagnostic work up should include relevant clinical history, physical examination, proper imaging protocol and urine analysis for bacteriological examination. Limited per vaginal examination to rule out labial adhesions and other local anatomical abnormalities leading to development of VVR would be valuable [7]. Imaging protocol should include dynamic sonography during micturition in full bladder which demonstrates fluid-filled vaginal mass and its complete resolution on postvoid scan. Voiding cystourethrogram may be performed to confirm the above findings and to rule out vesicoureteral reflux, wide bladder neck, spinning top urethra which are associated with functional voiding disturbances which could be a cause of recurrent UTI [8,9] (Figure 3). Additional diagnostic investigations like Intravenous Urography (Figure 3 and Figure 4), CT urography and MRI studies are useful to rule out urogenital tract anomalies like Vesicovaginal fistula (Figure 5), ectopic ureter and any associated Mullerian duct anomalies. Management includes treatment of UTI, parenteral education regarding the condition and behavioural therapy with proper toilet training for the patients where it is advised for frequent urination, avoiding with holding of urine for long hours and maintenance of voiding dairy.
Conclusion
Paediatricians and radiologists should be aware of this less recognised entity of VVR and proper imaging protocol is required for correct diagnosis. Disappearance of vaginal collection of any size following micturition in the absence of other structural abnormalities nearly always clinches the diagnosis of Vesicovaginal reflux with non-obstructive urocolpos. In school going children with VVR, behavioural modifications, parental education and suitable instructions to the school authorities regarding the toilet training of the patient reduces the occurrence of UTI and other distressing symptoms.
Acknowledgment
Department of Paediatrics of both Hospitals.
References
- Snyder EM, Nguyen RA, Young KJ, Coley BD (2007) Vesicovaginal reflux mimicking obstructive hydrocolpos. J Ultrasound Med 26: 1781-1784.
- Schaffer RM, Taylor C, Haller JO, Friedman AP, Shih YH (1983) Nonobstructive hydrocolpos: sonographic appearance and differential diagnosis. Radiology 149: 273-278.
- Davis LA, Chumley WF (1966) The frequency of vaginal reflux during micturition--its possible importance to the interpretation of urine cultures. Pediatrics 38: 293-294.
- Stannard MW, Lebowitz RL (1978) Urography in the child who wets. AJR Am J Roentgenol 130: 959-962.
- Capraro VJ, Greenberg H (1972) Adhesions of the labia minora. A study of 50 patients. Obstet Gynecol 39: 65-69.
- Szabó L, Lombay B, Borbás E, Bajusz I (2004) Videourodynamics in the diagnosis of urinary tract abnormalities in a single center. Pediatr Nephrol 19: 326-331.
- Warade M, Majid Y, Dayananda L, Gupta K (2009) Vesicovaginal reflux: A case report. Indian J Radiol Imaging 19: 235-237.
- Hausegger KA, Fotter R, Sorantin E, Schmidt P (1991) Urethral morphology and bladder instability. Pediatr Radiol 21: 278-280.
- Saxton HM, Borzyskowski M, Mundy AR, Vivian GC (1988) Spinning top urethra: not a normal variant. Radiology 168: 147-150.