Case Report
Neuroimaging of a Rare Congenital Disorder- Moebius Syndrome
Joshi A1, Benjwal G2*, Sharma G2 and Kala P2
1Department of Anatomy, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Dehradun, Uttarakhand, India
2Department of Radiodiagnosis, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Dehradun, Uttarakhand, India
*Corresponding author:Gaurav Benjwal, Department of Radiodiagnosis, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Dehradun, Uttarakhand, India. Email id: grv_22@ymail.com
Copyright: ©2025 Joshi A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Information:Submission:14/03/2025; Accepted: 07/04/2025; Published: 12/04/2025
Abstract
Moebius syndrome(MBS) is a rare congenital neuromuscular disorder of the unilateral or bilateral sixth and seventh cranial nerve. It is mostly a clinical diagnosis but neuroimaging can aid in detecting its salient features.
This case report is a documentation of Magnetic resonance (MR) findings of a 9-year-old female diagnosed with MBS. Neuroimaging showed bilateral hypoplastic abducens nerves and bilaterally absent facial nerves with associated ventriculomegaly, hippocampal malrotation, and midbrain malformation.
Thus, neuroimaging using magnetic resonance can be used to capture the radiological features of MBS.
This case report is a documentation of Magnetic resonance (MR) findings of a 9-year-old female diagnosed with MBS. Neuroimaging showed bilateral hypoplastic abducens nerves and bilaterally absent facial nerves with associated ventriculomegaly, hippocampal malrotation, and midbrain malformation.
Thus, neuroimaging using magnetic resonance can be used to capture the radiological features of MBS.
Keywords:Moebius Syndrome; MRI; Facial Nerve; Abducens Nerve; Ventriculomegaly
Introduction
Moebius syndrome (MBS) is a rare congenital neuromuscular
disorder characterized by non-progressive weakness of the sixth (VI)
and seventh (VII) cranial nerves, leading to ophthalmoplegia and
facial paralysis. First described by Von Graefe and Saemisch in 1880
and later confirmed by Paul Julius Moebius in 1888, the prevalence of
the syndrome is approximately 1 in 25,000 live births, with no gender
predilection and mostly sporadic cases [1]. Since it can resemble
several other neuromuscular conditions, neuroimaging can aid in
better differentiating it from its clinical mimics.
Here, we report the case of a 9-year-old girl diagnosed with Moebius syndrome, focusing on its characteristic MRI findings.
Here, we report the case of a 9-year-old girl diagnosed with Moebius syndrome, focusing on its characteristic MRI findings.
Case Report
A 9year old girl presented to the pediatric OPD with complaints
of the inability to move both eyes laterally and slurred speech. She
lacked facial expressions since birth and had recurrent episodes of
corneal ulcers, as informed by her parents. She also had drooling
of saliva from the corners of her mouth since birth. On detailed
physical examination, the patient had bilateral deficits of VI, VII and
XII cranial nerves evidenced by the inability to move both her eyes
laterally, bilateral absence of frowning, cheek blowing, proper eye
closure, nasolabial folds and facial expressions and upward deviation
of tongue respectively.
Multiplanar MR imaging of the cranium was done on a 1.5
Tesla magnet (SIEMENS 1.5T MAGNETOM) using a dedicated
head coil. T1, T2 weighted images were obtained in axial, sagittal
and coronal planes using Spin Echo and Gradient Echo sequences.
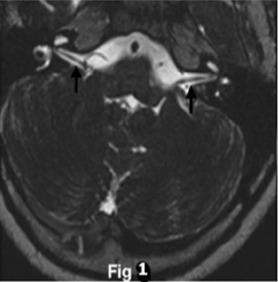
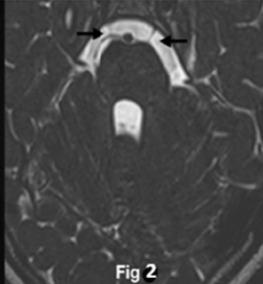
Constructive Interference in Steady State (CISS) sequence showed
bilaterally absent cranial nerves VII [Figure 1] and thinned-out
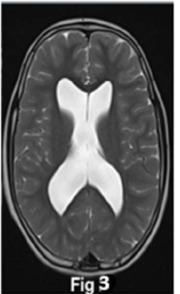
hypoplastic cranial nerves VI [Figure 2]. Ventriculomegaly [Figure 3] with predominantly prominent frontal horn without obstructive
hydrocephalus was noted. Partial fusion of thalami was seen along
a narrow band with mild reduction of the interpeduncular cistern
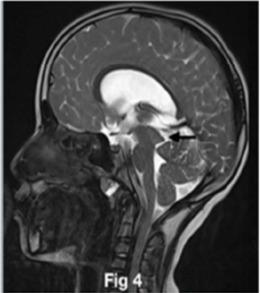
diameter.T2W sagittal images showed Tectal beaking [Figure 4] and
absent facial colliculus with resultant straightening of the fourth
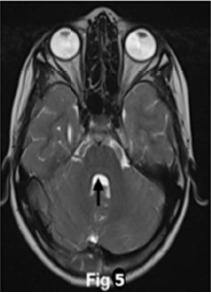
ventricle’s floor [Figure 5].
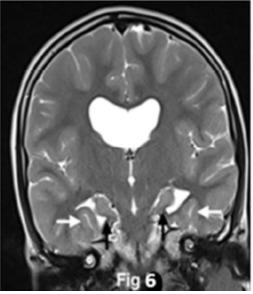
T2W coronal inversion recovery sequence demonstrated
malrotation of bilateral hippocampus [Figure 6] with deep and vertical
collateral sulcus. The scan showed no calcifications or hemorrhages.
The brain parenchyma, brainstem and cerebellum were normal
Figure 1:Enlarged image from 3D CISS sequence demonstrating
the absence of facial (Cranial nerve VII) nerves bilaterally with single
nerve (vestibulocochlear nerve; black arrows) coursing through bilateral
cerebellopontine angle cisterns and internal acoustic meatuses supplying
bilateral inner ear structures.
Figure 2:Enlarged image from 3D CISS sequence demonstrating thinning
and reduced calibre of bilateral abducens nerves in the prepontine cistern
(black arrows).
Figure 5:Axial T2W image displaying fourth ventricle floor straightening
(black arrow) due to absence of facial colliculus.
Figure 6:Coronal T2W image demonstrating bilateral hippocampal
malrotation (black arrows) associated with the vertical orientation of the
collateral sulci bilaterally (white arrows).
Informed consent, including permission about potential
publication in a scientific journal was obtained from the father of the
patient involved in the study.
Discussion
MBS develops due to faulty embryogenesis of the mesencephalon
and rhombencephalon[2]. Histopathological evaluation identifies the
primary pathology in the pontine tegmentum [3], where the nuclei of
the VI cranial nerve and the posterior facial colliculus are located.
Among the various diagnostic criteria for MBS, Kumar et al. outlined the following: (a) partial or complete VII nerve paralysis, (b) associated limb defects such as syndactyly, brachydactyly, absent
Among the various diagnostic criteria for MBS, Kumar et al. outlined the following: (a) partial or complete VII nerve paralysis, (b) associated limb defects such as syndactyly, brachydactyly, absent
digits, or talipes, (c) unilateral or bilateral cranial nerve palsies
(including VI, XII, IX, and X), and (d) potential orofacial, ear, and
musculoskeletal deformities [3]. Meanwhile, Verzijl et al. emphasized
facial palsy and impaired ocular abduction as key diagnostic features.
[3] The present case satisfies both criteria.
Other cranial nerves frequently involved in MBS include V,
IX, X, XI, and XII ,[4] with cranial nerve XII being the third most
commonly affected.[3] Verzijl et al. proposed that MBS may
arise from either a genetic defect affecting the VII nerve nuclei or
intrauterine environmental and mechanical factors that disrupt
brainstem vascularity.[3] However, Cocaine and Misoprostol use
during pregnancy have also been associated with MBS,[5,6] which
suggests that MBS is a possible teratogenic effect of these drugs.
While MBS is primarily diagnosed clinically, neuroimaging
modalities such as MRI allows direct imaging of cranial nerves and
extraocular muscles. The MRI findings in this case align with those
reported by Matsui et al. ,[7] showing ventriculomegaly without
features of obstructive hydrocephalus. However, Matsui et al. did
identify hydrocephalus in some patients with ventriculomegaly.
In contrast, a cross-sectional study by Herrera et al. [8] found
ventriculomegaly and hydrocephalus in only a few cases. Cerebral
aqueductal stenosis was identified as the underlying cause of
obstructive hydrocephalus in both studies.
The possible cause of ventriculomegaly without obstructive
hydrocephalus in MBS can be white matter volume loss which can
manifest as prominent frontal horns of lateral ventricle in the present
case and other researches.[7,8]
Brainstem and cerebellar hypoplasia are commonly reported in MBS;[1,3,9] however, neuroimaging in this case revealed normal appearances of both structures. Infratentorial anomalies, including mesencephalic malformations with a reduced interpeduncular cistern diameter and tectal breaking, were noted in this case, consistent with the findings of Volpe et al. [10]
Thalamic fusion has been documented in MBS, with an established association between thalamic fusion and agenesis of the septum pellucidum, indicating a mild form of lobar holoprosencephaly.[8] The neuroimaging findings in this case corroborate this association. The absence of the facial colliculus, a characteristic feature of MBS, results in a straightened floor of the fourth ventricle, a finding observed in this case. However, some studies describe the floor of the fourth ventricle as horseshoe-shaped.[3,8]
Brainstem and cerebellar hypoplasia are commonly reported in MBS;[1,3,9] however, neuroimaging in this case revealed normal appearances of both structures. Infratentorial anomalies, including mesencephalic malformations with a reduced interpeduncular cistern diameter and tectal breaking, were noted in this case, consistent with the findings of Volpe et al. [10]
Thalamic fusion has been documented in MBS, with an established association between thalamic fusion and agenesis of the septum pellucidum, indicating a mild form of lobar holoprosencephaly.[8] The neuroimaging findings in this case corroborate this association. The absence of the facial colliculus, a characteristic feature of MBS, results in a straightened floor of the fourth ventricle, a finding observed in this case. However, some studies describe the floor of the fourth ventricle as horseshoe-shaped.[3,8]
Hippocampal malrotation, as noted in this case, has also been
reported in some subjects in a cross-sectional study by Herrera et al.
[8]Calcification in the pontine region housing the VI nerve nuclei has
been documented in MBS,[3,10]although it was not observed in this
case.
The management of MBS is primarily supportive and
symptomatic, requiring long-term multidisciplinary care, including
physical, psychological, speech, and occupational therapy.
Conclusion/Summary
Neuroimaginging MBS particularly MRI shows bilateral
hypoplastic abducens nerves and absent facial nerves with associated
ventriculomegaly, hippocampal malrotation, and midbrain
malformation. Thus, MRI using the CISS sequence can play an
important role in evaluating brainstem and associated abnormalities
in MBS which can be helpful for clinicians to differentiate it from
other congenital neuromuscular disorders.
Acknowledgement
The work was conducted in the Department of Radiodiagnosis,
Himalayan Institute of Medical Sciences, Dehradun, India. We
appreciate the work of all the authors and staff involved in generating
this case report.