Research Article
Evaluation of the Ultrasound Doppler Parameters of Foetal Vessels in Pregnancies with Suspected Intrauterine Growth Retardation: A Prospective Study
Metya S1* and Madan M2
1Post Graduate Trainee, West Bengal University of Health Sciences, Kolkata, India
2Professor of Radiology, West Bengal University of Health Sciences, Kolkata India
2Professor of Radiology, West Bengal University of Health Sciences, Kolkata India
*Corresponding author:Subha Metya, Post Graduate Trainee, West Bengal University of Health Sciences, Kolkata, India-mail Id: subhametya007@gmail.com
Copyright:©2024 Metya S, et al. This is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Information:Submission: 07/01/2024; Accepted: 23/02/2024; Published: 28/02/2024
Abstract
Objective:This study investigates fetal hemodynamic changes in Intrauterine Growth Retardation (IUGR), evaluates Dopplerchanges in fetal arteries, and examines their association with adverse perinatal outcomes.
Materials and Methods:A prospective observational study in tertiary care medical college &hospital (Nov 2022 - Jun 2023) included 50 IUGR-suspected pregnancies. Criteria included singleton pregnancies over 24 weeks gestation with fetal weight below the 10th percentile. Doppler indices measured were pulsatility index (PI) for the umbilical artery, middle cerebral artery, and thoracic aorta, along with cerebroplacental ratio. Outcomes assessed were gestational age at delivery, cesarean section, birth weight, NICU admissions, and perinatal deaths.
Results:Abnormal PIs were found in 34% (umbilical artery), 38% (middle cerebral artery), and 26% (thoracic aorta) of cases. An abnormal cerebroplacental ratio was observed in 13 cases. There was a significant link between abnormal Doppler findings and increased cesarean sections, NICU admissions, and perinatal deaths, with the highest risks associated with abnormal cerebroplacental ratios and reversed end-diastolic flow in the umbilical artery.
Conclusion:Abnormal Doppler indices in the middle cerebral artery, umbilical artery, and thoracic aorta significantly correlate with adverse perinatal outcomes in IUGR pregnancies. The highest association with adverse outcomes, including perinatal death, is seen with abnormal cerebroplacental ratios. This study highlights the critical role of Doppler ultrasonography in managing IUGR pregnancies, suggesting the need for further large-scale studies.
Materials and Methods:A prospective observational study in tertiary care medical college &hospital (Nov 2022 - Jun 2023) included 50 IUGR-suspected pregnancies. Criteria included singleton pregnancies over 24 weeks gestation with fetal weight below the 10th percentile. Doppler indices measured were pulsatility index (PI) for the umbilical artery, middle cerebral artery, and thoracic aorta, along with cerebroplacental ratio. Outcomes assessed were gestational age at delivery, cesarean section, birth weight, NICU admissions, and perinatal deaths.
Results:Abnormal PIs were found in 34% (umbilical artery), 38% (middle cerebral artery), and 26% (thoracic aorta) of cases. An abnormal cerebroplacental ratio was observed in 13 cases. There was a significant link between abnormal Doppler findings and increased cesarean sections, NICU admissions, and perinatal deaths, with the highest risks associated with abnormal cerebroplacental ratios and reversed end-diastolic flow in the umbilical artery.
Conclusion:Abnormal Doppler indices in the middle cerebral artery, umbilical artery, and thoracic aorta significantly correlate with adverse perinatal outcomes in IUGR pregnancies. The highest association with adverse outcomes, including perinatal death, is seen with abnormal cerebroplacental ratios. This study highlights the critical role of Doppler ultrasonography in managing IUGR pregnancies, suggesting the need for further large-scale studies.
Keywords:Intrauterine Growth Retardation; Doppler Ultrasonography; Perinatal Outcomes; Cerebroplacental Ratio
Introduction
Intrauterine Growth Retardation is defined as foetal weight
below the10th percentile for gestational age [1]. While often used
interchangeably, IUGR and Small for Gestational Age (SGA) are not
synonymous. SGA includes a broader spectrum: foetuses with IUGR,
constitutionally small but healthy foetuses, and cases misdiagnosed as
small [2].Unlike most SGA cases, IUGR foetuses face increased risks
of serious conditions such as hypoxemia, acidemia, and intrauterine
foetal demise [2].The incidence of IUGR varies from 3-10% of all live
births, increasing in specific groups like stillborn infants and women
with a history of hypertension or IUGR [1]. IUGR in India is a major
cause of low birth weight babies, posing significant challenges to
maternal and child health and socio economic conditions [3].The
prime target in antenatal care is the early identification of IUGR
to prevent adverse outcomes, emphasizing the need for accurate
diagnostic methods [4].Since the 1960s, ultrasonography, especially
fetal biometry, has been essential in assessing fetal size and growth,
surpassing traditional methods [5].Colour Doppler Ultrasound has
been pivotal in studying been pivotal in studying foetal hemodynamic,
providing insights into uteroplacental insufficiency and fetal acidbase
base status [2].Changes in the Doppler flow velocity waveform
of the umbilical artery, middle cerebral artery, and thoracic aorta are
strong predictors of adverse perinatal outcomes. These include timing
of delivery, caesarean sections for fetal distress, NICU admissions,
and early complications in newborns like necrotizing enterocolitis
and hypoxic-ischemic encephalopathy [4].Clinical Implications:
The ability to predict such outcomes underscores the importance of
incorporating Doppler ultrasound in routine prenatal screening for
IUGR, aiding in timely intervention and management[6].
Aim and Objectives
The research sought to delve into the underlying mechanisms of
fetal hemodynamic alterations in Intrauterine Growth Restriction
(IUGR), examining Doppler shifts within the fetal arterial network,
with a specific focus on the middle cerebral artery, umbilical artery,
and thoracic aorta. Additionally, it aimed to uncover potential
links between Doppler irregularities and unfavorable perinatal
consequences associated with IUGR. Key objectives encompassed
the computation of pulsatility index (PI) values across these arterial
sites, scrutiny of variations in end-diastolic flow patterns, analysis of
perinatal outcomes among participants, and elucidation of potential
correlations between Doppler anomalies and adverse perinatal events.
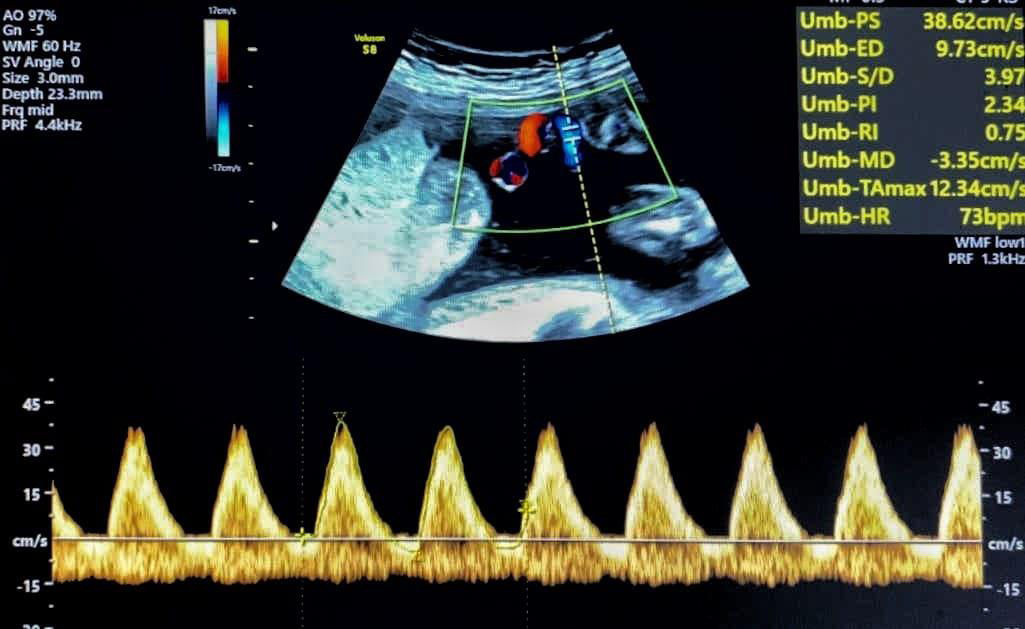
Materials and Methods
The research took place at the Radiology Department of IQ
City Medical College & Hospital, spanning from November 2022
to June 2023. The study focused on expectant mothers suspected of
Intrauterine Growth Restriction (IUGR), referred by the Department
of Gynecology and Obstetrics. Eligible participants met criteria
including carrying a single fetus, having a gestational age of at
least 24 weeks verified by previous ultrasonography, and exhibiting
fetal weight below the 10th percentile or a head circumference
to abdominal circumference (HC/AC) ratio exceeding 1.20 as
determined by ultrasonography. Instances of significant congenital
or chromosomal anomalies in pregnancies were excluded. The study
adopted a prospective observational approach within a hospital
setting, enrolling a sample of 50 cases chosen via systematic random
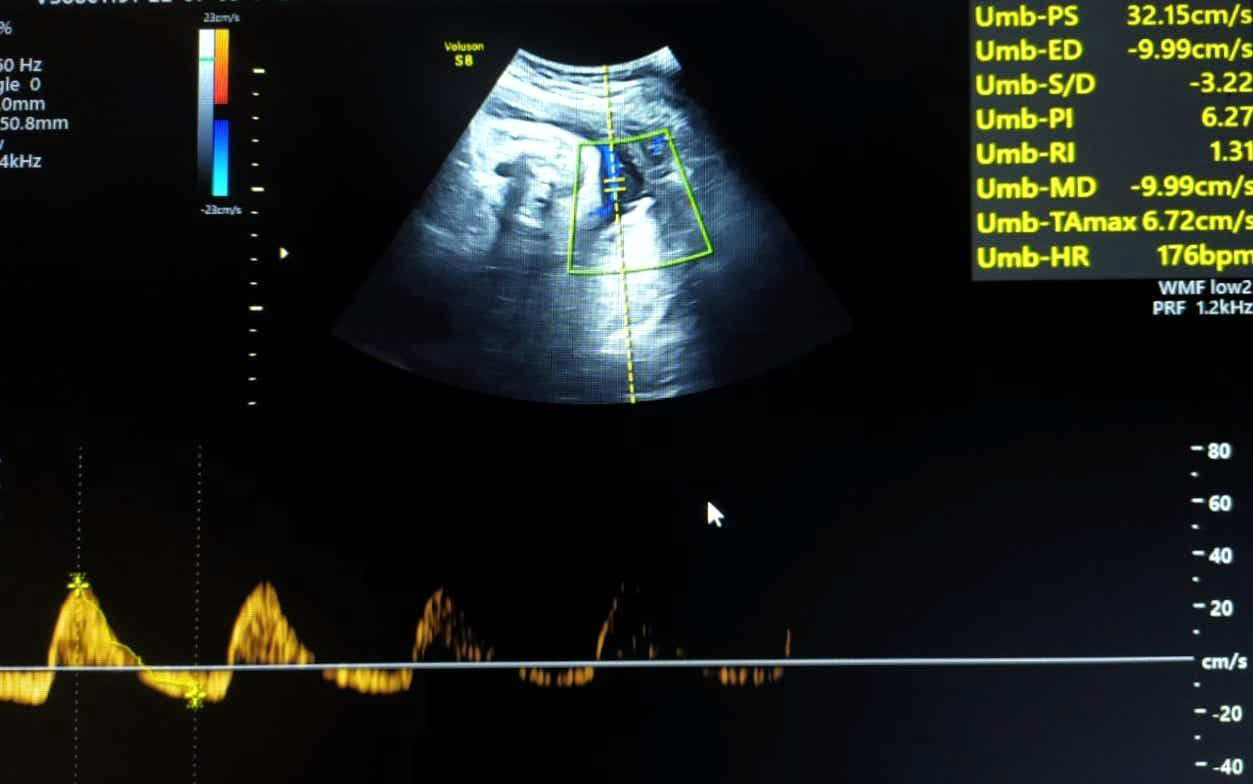
sampling. Ultrasound assessments utilized the GE Volusion S8
system, incorporating a curved-array transducer (3.5-5.0 MHz),
adjustable wall filter settings (50-100 Hz), and sample volume
adjustments to encompass vessel diameters adequately. Before
participation, each patient provided informed consent after receiving
detailed explanations regarding the study’s objectives, methodologies,
and potential repercussions.
Fetuses included in the research exhibited estimated weights
below the 10th percentile corresponding to their gestational age.
Statistical analysis was performed using the “Epi info version
7.1.4.0” software published by WHO. We grouped cases according
to abnormal and normal PI and EDF for each vessel and calculated
the number of adverse perinatal outcomes (cesarean section,
NICU admission, and perinatal death) in each group. The Z test
for proportions was used to determine the strength of association
between the outcomes and Doppler abnormalities, considering a
p-value less than 0.05 as significant.
Results
Throughout our research, which spanned from November 2022
to June 2023 at IQ City Medical College & Hospital, we conducted
fetal biometry assessments on approximately 200 fetuses. After
meticulous screening, 50 fetuses were deemed eligible for inclusion
based on stringent criteria. Noteworthy is that all these selected fetuses
exhibited an estimated weight below the 10th percentile for their
gestational age. It is intriguing to observe that only 3 (6%) of these
fetuses displayed a head circumference to abdominal circumference
ratio exceeding 1.2.
We found that 16% of women had preexisting conditions, with
8% of cases involving heart disease. Additionally, 28% had significant
medical histories, with 14% reporting a history of spontaneous
abortion. Notably, instances of Intrauterine Fetal Death (IUFD) and
perinatal death were each noted once. Throughout the study duration,
40% of these women faced at least one pregnancy complication, with
oligohydramnios being the most common, affecting 28% of cases.
The gestational age of the fetuses averaged 32.5 weeks during
the Doppler ultrasound examination, approximately 3.5 weeks less
than the mean clinical age calculated from the Last Menstrual Period
(LMP) or earlier ultrasound scans. All fetuses were estimated to weigh
below the 10th percentile for their gestational age, with 44% below the
3rd percentile. The mean estimated fetal weight was 1980 grams.
Our Doppler ultrasound study revealed abnormalities in 58%
of the fetuses, particularly in the pulsatility index (PI). Abnormal
PI values were observed in 19 cases (65% of total abnormalities) in
the middle cerebral artery (MCA), 17 cases (58%) in the umbilical
artery (UA), and 13 cases (45%) in the thoracic aorta (TA). The
cerebroplacental ratio was also found to be abnormal (less than 1) in
13 cases (45% of total abnormalities). Remarkably, 16 cases exhibited
abnormalities in more than one vessel, including both MCA and UA,
MCA and TA, UA and TA in 4 cases each, and all three vessels in
another 4 cases. Isolated abnormalities in MCA, UA, and TA were
found in 7, 5, and 1 case(s), respectively.
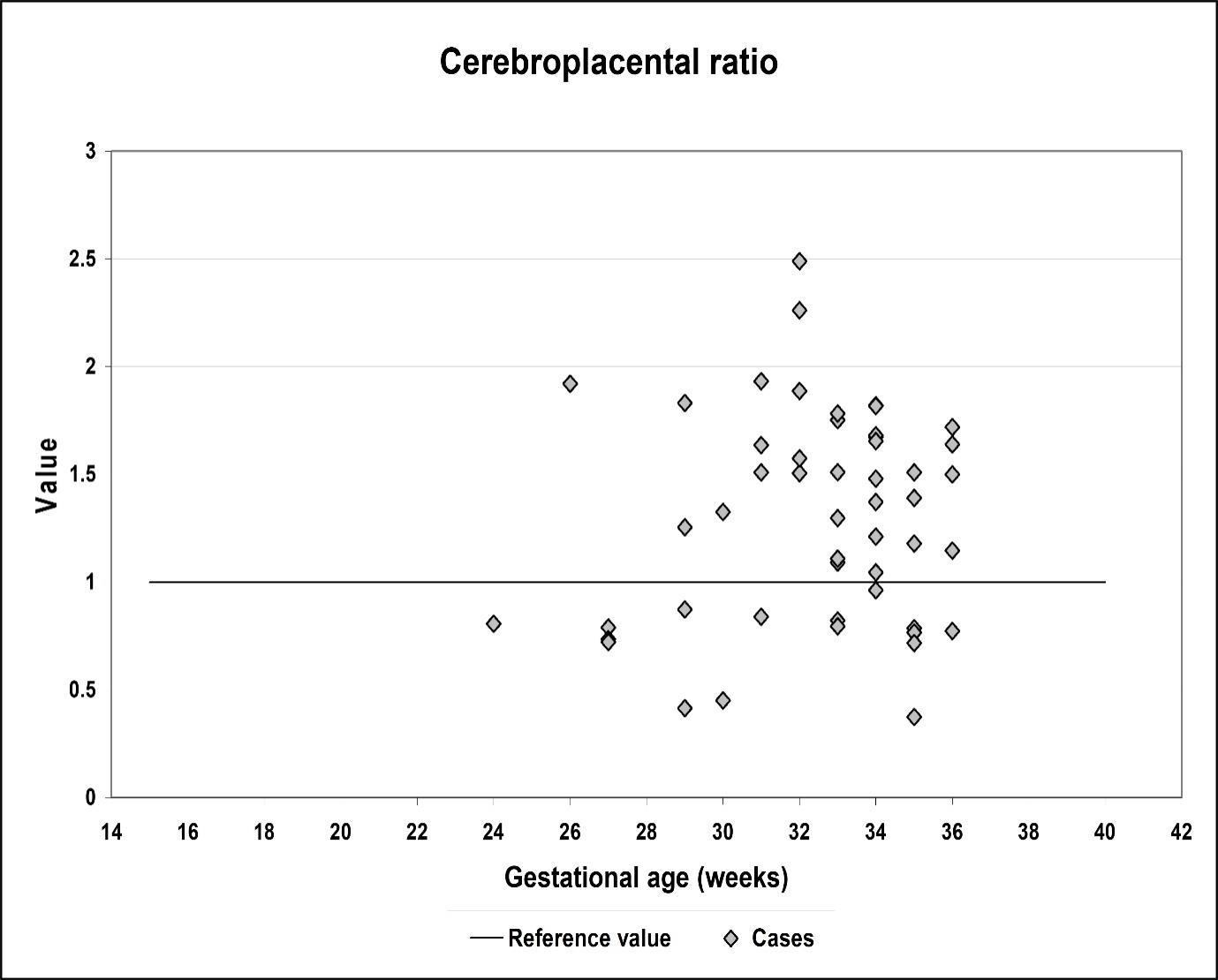
Figure 1:Diagram showing the ratio of MCA PI to UA PI in 50 fetuses
examined plotted against gestational age at the time of Doppler examination.
Normal reference value is 1 throughout the gestational period. Values less
than 1 are abnormal (n = 13).
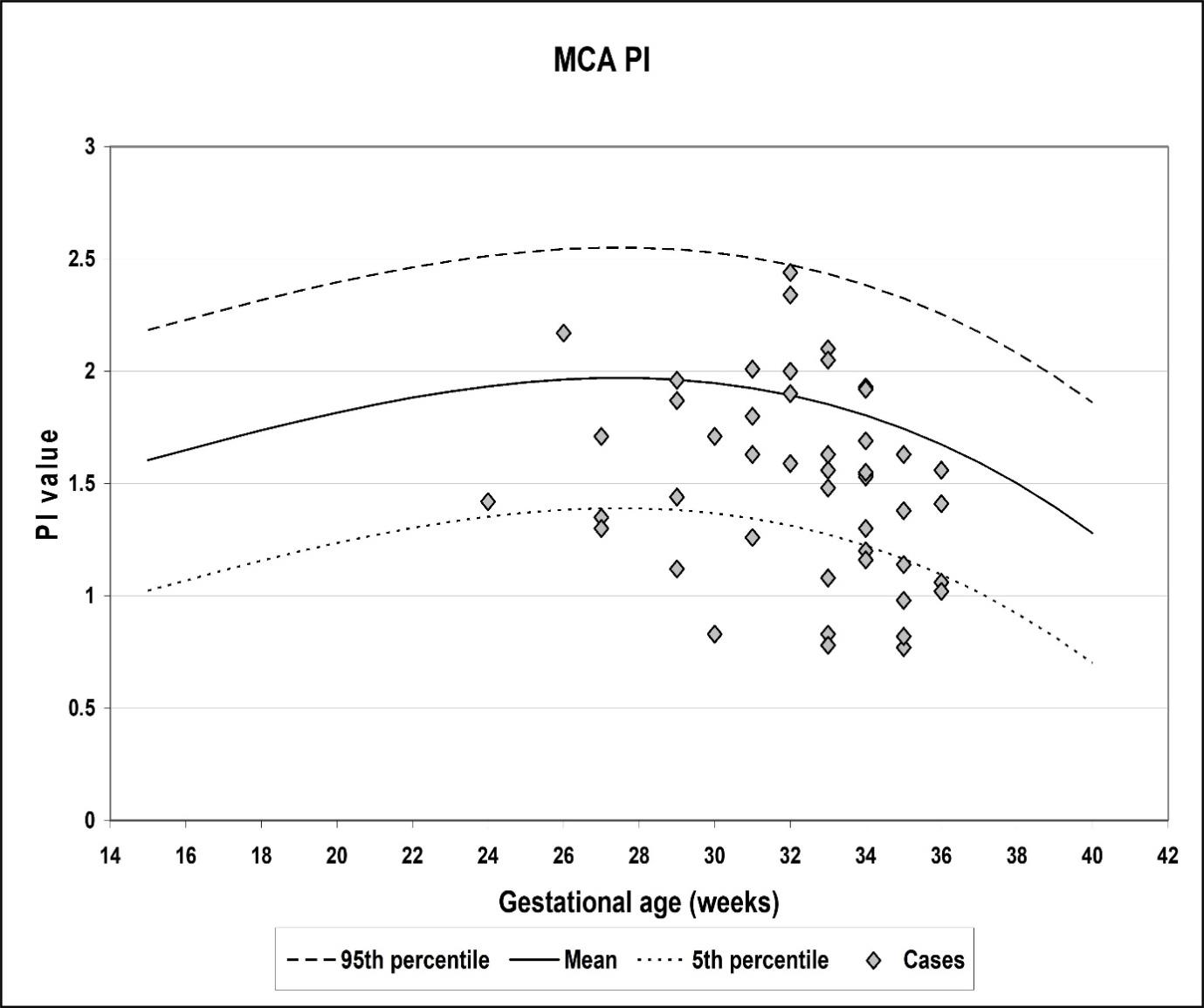
Figure 2:Diagram showing PI values obtained from MCA in 50 fetuses
examined plotted against gestational age at the time of Doppler examination.
Normal ranges for gestational age are shown as mean, 5th, and 95th
percentiles. Values that fell below the 5th percentile are abnormal (n = 19).
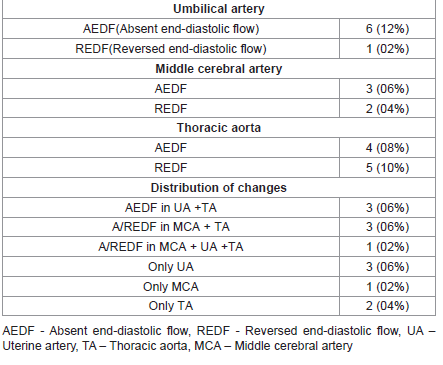
Moreover, qualitative changes in the flow velocity waveform were
observed in 13 cases (26%), characterized by absent or reversed enddiastolic
flow (EDF). These EDF changes were noted in MCA in 4
cases, UA in 7 cases, and TA in 10 cases. In 7 cases, EDF changes
were observed in more than one vessel, including both MCA and
TA in 3 cases, and both UA and TA in another 3 cases. One case
exhibited changes in all three vessels. All cases with EDF changes
were associated with abnormal PI values.
The perinatal outcomes of the 50 fetuses examined were
meticulously documented. The mean gestational age at delivery for
all cases was 34.8 weeks, with an overall mean birth weight of 2271
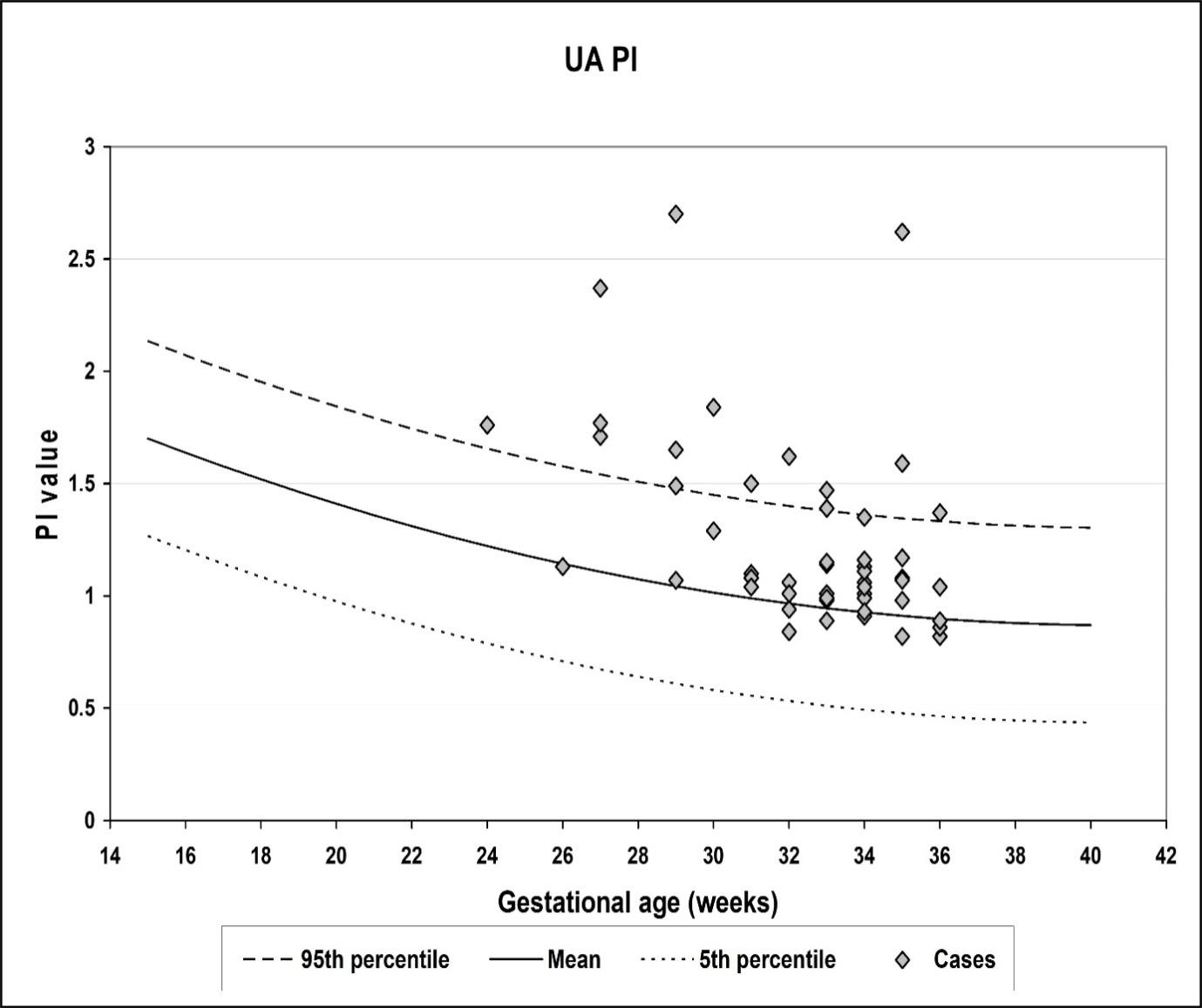
Figure 3:Diagram showing PI values obtained from UA in 50 fetuses
examined plotted against gestational age at the time of Doppler examination.
Normal ranges for gestational age are shown as mean, 5th, and 95th
percentiles. Values that fell above the 95th percentile are abnormal (n = 17).
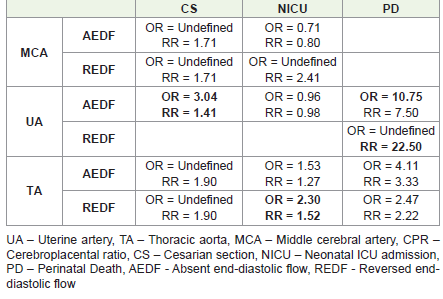
Table 1:End-diastolic flow changes in umbilical artery, middle cerebral artery and
thoracic aorta in cases of suspected IUGR
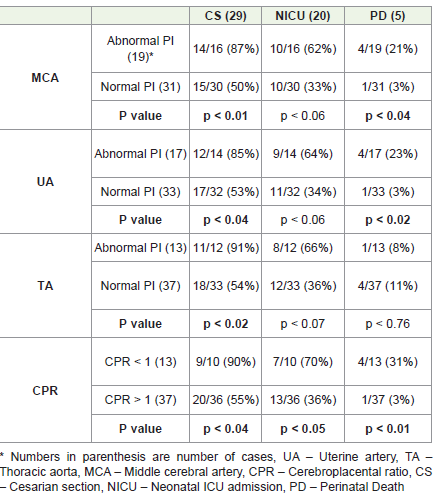
Table 2:Showing the strength of association between the abnormal PI values
for each vessel and abnormal cerebroplacental ratio with adverse perinatal
outcomes.
grams. Notably, 68% of the babies born weighed less than 2500 grams.
The mean gestational age at delivery and mean birth weight were
significantly lower in the abnormal PI group (33.8 weeks and 1821
grams, respectively) compared to the normal PI group (35.4 weeks
and 2363 grams). There were 4 stillbirths and 46 live births, with
29 cases (63% of liveborn) requiring cesarean sections due to fetal
distress. Among the 46 liveborn neonates, 20 (43%) were admitted to
the neonatal intensive care unit (NICU), and one neonate succumbed
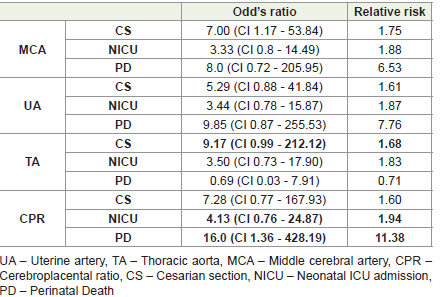
Table 3:Showing the Odd’s ratio and relative risk of adverse perinatal outcome
for abnormal PI values for each vessel examined.
Table 4:Showing the Odd’s ratio and relative risk of adverse perinatal outcome
for abnormal EDF changes for each vessel examined
during the neonatal period. The total number of cases exhibiting at
least one adverse perinatal outcome was 34. Among the cesarean
deliveries, 17 neonates also required NICU admission.
Our findings revealed significant associations between abnormal
MCA PI and cesarean section for fetal distress (p < 0.01) and perinatal
death (p < 0.04). Similarly, abnormal UA PI was linked to cesarean
section (p < 0.04) and perinatal death (p < 0.02). Abnormal TA PI
was significantly associated with cesarean section for fetal distress (p
< 0.02). Additionally, an abnormal cerebroplacental ratio (less than
1) was correlated with cesarean section for fetal distress (p < 0.04),
NICU admission (p < 0.05), and perinatal death (p < 0.01).
Odds ratios (OR) and Relative Risks (RR) were calculated
for each abnormal PI, indicating that abnormal PI in all vessels
identified women at increased risk of adverse perinatal outcomes. The
highest risk of cesarean section for fetal distress was associated with
abnormal TA PI (OR = 9.17; RR = 1.68), followed by an abnormal
cerebroplacental ratio (OR = 7.28; RR = 1.60). The highest risk of
NICU admission was linked to an abnormal cerebroplacental ratio
(OR = 4.13; RR = 1.94), followed by an abnormal TA PI (OR = 3.50;
RR = 1.83). The greatest risk of perinatal death was observed with an
abnormal cerebroplacental ratio (OR = 16.0; RR = 11.38), followed by
an abnormal UA PI (OR = 9.85; RR = 7.76).
Discussion
Our study’s results are consistent with or exceed the findings of
similar studies in the field, such as those conducted by Baschat et al
[2], Figueras et al [7], Cruz-Martinez et al [8], Khalil et al [9], and Turan et al [10], in terms of odds ratio (OR) and sensitivity values for cerebroplacental ratio (CPR) and umbilical artery pulsatility index
(UA PI). These comparisons highlight the reliability and validity of
our results in the context of established research.
For instance, in the studies by Baschat et al [2] and Figueras et al
[7], the OR for perinatal death associated with CPR was 10.8 and 8.9,
respectively, with sensitivity values of 82% and 80%. In contrast, our
study demonstrated a higher OR of 16.0 for CPR, with a remarkable
sensitivity of 90%, indicating a stronger predictive value for adverse
perinatal outcomes.
Similarly, when comparing UA PI, our study’s OR of 9.85 and
sensitivity of 86.6% are either comparable or superior to those
reported in the aforementioned studies. For example, Khalil et al [9]
reported an OR of 3.8 and a sensitivity of 63% for UA PI, which are
lower than our findings. This suggests that our study’s parameters,
particularly CPR and UA PI, are effective indicators of potential
adverse perinatal outcomes.
Notably, our study also observed significant associations with
thoracic aorta pulsatility index (TA PI) and end-diastolic flow (EDF)
changes, further enhancing the comprehensive understanding of
Doppler parameters in the assessment of fetuses at risk of adverse
outcomes.
However, it is important to acknowledge the limitations of our
study. These include a relatively small sample size, which may affect
the generalizability of the results. Additionally, the lack of ductus
venosus pulsatility index (DV PI) measurement and the absence
of long-term follow-up data on neonates limit the scope of our
findings. Future research with larger sample sizes, inclusion of DV PI
measurements, and extended follow-up periods would be valuable in
validating and expanding upon our results.
Ethical Approval:
The study followed the ethical principles of the Declaration of
Helsinki and received approval from the IQ City Medical College &
Hospital’s Institutional Ethics Committee. All participants gave their
informed consent after learning about the study’s aims, procedures,
and possible hazards. The study guaranteed confidentiality to the
participants and let them know that they could quit the study anytime
without compromising their medical treatment. The study protected
participant privacy by anonymizing all data.